Abstracts
Orthodontic treatment with extraction of molars in adult patients is technically more complex due to a number of factors. In general, the space to be closed is greater than premolar spaces rendering critical anchorage and longer treatment time. Often such cases exhibit some degree of periodontal involvement due to patient age. Hence, the need for greater control over orthodontic mechanics to reduce the side effects of space closure. Therefore, good finishing results can be more difficult to achieve. Thus, the purpose of this article is to determine the reasons for molar extraction indications, describe different stages of orthodontic mechanics, and explain the issues involved in this kind of planning and treatment. Additionally, it aims at describing some treatments with molar extractions.
Angle Class I malocclusion; Tooth extraction; Corrective orthodontics
O tratamento ortodôntico com extração de molares em pacientes adultos é tecnicamente mais complexo, devido a inúmeros fatores. Em geral, o espaço a ser fechado é maior do que o espaço dos pré-molares e, por isso, a ancoragem é crítica e o tempo de tratamento mais longo. É comum esses casos apresentarem algum grau de comprometimento periodontal por causa da idade dos pacientes e, portanto, necessitam de maior controle da mecânica ortodôntica para reduzir os efeitos colaterais do fechamento do espaço. Por isso, bons resultados de finalização são mais difíceis de ser alcançados. Sendo assim, este artigo tem como objetivo apresentar as razões para a indicação de extração de molares nos tratamentos ortodônticos, as contraindicações, as diferentes fases da mecânica ortodôntica, esclarecer os fatores envolvidos nesse tipo de planejamento e tratamento e apresentar casos clínicos tratados com extração de molares.
Má oclusão Classe I de Angle; Extração dentária; Ortodontia Corretiva
SPECIAL ARTICLE
IMSc and PhD in Orthodontics, Federal University of Rio de Janeiro (UFRJ). Professor of Orthodontics, Estácio de Sá University. Diplomate of the Brazilian Board of Orthodontics and Dentofacial Orthopedics (BBO)
IIMSc in Orthodontics, Federal University of Rio de Janeiro (UFRJ). Diplomate of the Brazilian Board of Orthodontics and Dentofacial Orthopedics (BBO)
IIISpecialist in Orthodontics, Rio de Janeiro State University (UERJ)
IVSpecialist in Orthodontics, Gama Filho University
Contact address
ABSTRACT
Orthodontic treatment with extraction of molars in adult patients is technically more complex due to a number of factors. In general, the space to be closed is greater than premolar spaces rendering critical anchorage and longer treatment time. Often such cases exhibit some degree of periodontal involvement due to patient age. Hence, the need for greater control over orthodontic mechanics to reduce the side effects of space closure. Therefore, good finishing results can be more difficult to achieve. Thus, the purpose of this article is to determine the reasons for molar extraction indications, describe different stages of orthodontic mechanics, and explain the issues involved in this kind of planning and treatment. Additionally, it aims at describing some treatments with molar extractions.
Keywords: Angle Class I malocclusion. Tooth extraction. Corrective orthodontics.
INTRODUCTION
Nowadays, a significant number of adult patients seek orthodontic treatment. These patients often present with some degree of dental involvement, including the absence of one or more molars.
In cases involving lack of space for tooth alignment, protruding teeth or intra-arch asymmetry, where extraction of permanent teeth is indicated, impaired molars may become the first extraction option when premolars are in better condition.
Orthodontic treatment with first molar extraction in adult patients is technically more complex and a positive outcome may prove harder to be achieved because there is more space to be closed, anchorage is critical and besides these patients usually have some degree of periodontal involvement. Furthermore, treatment takes longer and requires greater control of orthodontic mechanics to reduce the side effects of space closure.
Second molar extraction aiming at creating space for first molar distalization is a viable alternative that should be considered in correcting Angle Class II malocclusion. It may also be indicated in some cases of third molar impaction.
Third molar extractions are indicated for several reasons, with impaction emerging as the most common. Impaction stems from a scarcity of space in the dental arches or an inadequate axis of eruption.
This article seeks to present the manifold reasons for extracting molars in orthodontic treatment and clarify the issues involved in this type of planning and treatment.
EXTRACTION OF FIRST PERMANENT MOLARS
Indications
Extraction of first permanent molars for orthodontic purposes is indicated in the presence of excessively extruded molars endodontically treated, with caries and/or extensive restorations, with marked periodontal involvement; and in orthodontically retreated cases presenting with Angle Class II malocclusion in the absence of four premolars. Molar extractions are also indicated in severe crowding in patients with a high mandibular plane angle and convex profile as the mesialization of posterior teeth facilitates the counterclockwise rotation of the mandible and helps in cases where molars are missing from the outset.1-4
Contraindications
Given the complexity of orthodontic treatment involving extraction of first permanent molars, some situations must be avoided in order to prevent treatment prognosis from becoming limitated. These extractions are not indicated for patients who do not present with crowding and feature a decreased lower face height. It may be better to align the upper and lower teeth and prepare them for the use of dentures, implants or transplants in the extraction sites. Neither are these extractions indicated in noncompliant patients - due to a lengthy treatment time - or in patients who have already undergone previous orthodontic treatment and present with root resorption and/or short roots. In patients with bruxism, molar extractions should be avoided due to occlusal interferences that occur during space closure, causing an overload of forces on posterior teeth.1-4
Diagnosis and planning
In the diagnostic phase, first molars need to be assessed with respect to their individual clinical condition and all restorative, periodontal and periapical issues should be addressed. In some cases, clinicians may detect problems that lead to the unilateral decision to remove the corresponding tooth on the opposite side of the arch, even if it is healthy.
In cases where a first molar extraction is indicated, the presence of third molars in the dental arch is of paramount importance, or at least there should be a high likelihood of eruption of third molars in the dental arches.
The size and anatomy of second and third molar roots must also be adequate as they undergo substantial movement and short roots may hinder this procedure.
In patients with increased lower face or severe crowding, if one or more first molars have poor prognosis, extraction of all first molars may be considered. When planning extractions, one should assess whether one or both first molars should be extracted. Treatment mechanics can also benefit from upper first molar extraction. If the upper first molars need to be extracted it is sometimes possible to avoid the extraction of lower first molars. The unilateral extraction of a first molar may cause midline shift during space closure. The loss of a premolar or molar on the opposite side helps to preserve the midlines.
In cases where the second molar has not erupted, the right time for first molar extraction can be defined in accordance with the need for space utilization. The sooner the first molar is extracted, the more challenging will be the repositioning of the second molar in order to occupy that space. If the space needs to be utilized it is advisable to wait for the eruption of the second molar. If the first molars are extracted after eruption of the second molars, as indicated by orthodontic treatment, it is necessary to ensure the anchorage of this tooth, place the orthodontic appliance and immediately start the movement to close space. This averts tip, rotation of teeth adjacent to the extraction site and bone narrowing in the extraction site.1,2,3
Another common situation involves the need to close edentulous spaces. Such need can emerge due to loss of first molars, mesial tip of the second and third molars, distal tip of premolars, extrusion of molars in the opposing arch, changes in the shape of the gums, with bone narrowing and formation of bone defects on the mesial side of second molars. Impact on the upper arch is usually not as severe as in the lower arch.3,4
The longer the time elapsed after extraction, the worse the sequelae and orthodontists are advised to have caution. Molars can be moved through edentulous areas. However, the amount of remaining bone should be noted.3,4
The ideal alveolar dimensions in order to succeed in closing first molar space is 6 mm or less in the mesiodistal direction and 7 mm in the buccolingual direction.3,4
If the patient does not fit these characteristics, one can resort to the techniques of bone regeneration, which have been widely used for orthodontic movement in areas with bone defects.6
Orthodontic movement in adults - compared to young adults - presents greater resistance and entails a greater likelihood of loss of alveolar bone crest height, gingival recession and root resorption, in addition to greater difficulty in maintaining the closed space, i.e., decreased stability.8
To reduce these effects, orthodontists must use an efficient mechanism to ensure delivery of light forces and increase the interval between activations so that the tissues involved have time to recover. This approach greatly increases treatment time.
Aware of the consequences brought about by this procedure, orthodontists should consider other alternatives such as molar uprighting, with space creation every time mesial movements can jeopardize the maintenance of molars in the dental arches.
Molar uprighting produces significant reduction in the depth of existing periodontal defects, with highly desirable changes in gingival architecture, space creation adequate for the placement of an implant or prosthetic elements, and parallelism of abutment teeth for a better distribution of masticatory forces on pontic elements.7-10
The space created by molar extraction can be used to attain a number of goals. In some treatments it is necessary that molars remain in position in the anteroposterior direction, while the anterior teeth occupy the entire extraction space. In others, molars may drift mesially up to half the space, or even the entire space. There are also situations in which extraction spaces are used to establish intra-arch symmetry and correction of dental midlines, thus requiring asymmetric space closure. These different needs may render the case more complex mechanically and increase treatment time.
Anchorage loss occurs more easily in the upper arch and, therefore, when one needs to utilize the space created with extraction of the first molar to dilute crowding or even retract anterior teeth, one should establish appropriate anchorage mechanisms. In cases where there is no patient cooperation, but the patient agrees with skeletal anchorage, this is the best option to avoid anchorage loss.
Stages of orthodontic mechanics
Placement of the orthodontic appliance must be complete and include third molars if possible, starting with the initial alignment and leveling phase. Orthodontic auxiliaries should be placed on second molars so that during alignment and leveling tooth roots are tipped back mesially. This procedure seeks to accomplish parallelism between the roots of second molars and premolars during space closure. Attachments can also be positioned mesially on second molar crowns to reduce a rotation tendency when closing spaces.
In the alignment and leveling phase one can use a sequence of up to 0.018 x 0.025-in cross-section nickel-titanium wires, which can be used when molars are tipped lingually. Ideally, starting with round 0.018-in wires, steel wires should be used in coordination in the upper and lower arches. One is advised to avoid extending the initial archwires (0.012-in and 0.014-in) as far as the second and third molars to avert disrupting the region between the second premolar and second molar due to the large interbracket space present in the chewing area.
In cases with severe crowding, the use of archwires encompassing all teeth in the alignment and leveling phase will cause anterior teeth to protrude. If this is intended, small distal movements of the premolars and canines should be performed during the early stages of treatment in order to facilitate the alignment of anterior teeth. Distalization of these teeth can also be accomplished using segmented archwires with loops.
The space closure phase should only be initiated after full alignment and leveling of the dental arches.
During space closure one seeks to perform a bodily movement of the teeth, avoiding any side effects during movement, such as uncontrolled tipping and rotation of the molars, unwanted loss of anchorage, treatment lengthening, excessive incisor uprighting, increased overbite and even external root resorption.
In order for the posterior teeth to remain in their original position (steady anteroposterior position), it is necessary to use adequate anchorage, such as a Nance button, headgear or a mini-implant. The type of anchorage choice should be consistent with the patient's compliance profile. When using straight archwires in the lower arch, the maintenance of anchored posterior teeth can be achieved with tight omega loops and Class III elastics supported by the headgear on a delta loop in the lower canine region, or even by bracket hooks positioned on the lower canine teeth. This procedure is performed during the stage of premolar distalization. In the canine and incisor retraction phase the elastic can be supported directly by the retraction loop. In this type of mechanics, the premolars are distalized tooth after tooth with elastomeric chains. To reduce friction teeth may be distalized when using a 0.018-in archwire, and to reduce the possibility of rotation one can also use elastomeric chains lingually, which results in a binary system.
Since the extraction space is large and wire deformation is common in these regions, sliding mechanics cannot provide the desired efficacy. Segmented arches offer great advantages such as the elimination of friction and rotations, provided that one has control over this technique.
Special attention should be given to asymmetric cases, where it may be necessary to use mechanics comprising Class II elastics on one side and Class III elastics on the other side. Another option would be to use skeletal anchorage placed on different points of the dental arch.11
An ideal orthodontic appliance should deliver a relatively continuous force across a long distance. Therefore, it should feature a low load/deflection ratio and a wide activation range. To this end, it is essential that one be aware of the load/deflection ratio of the loop being used. Loops with a very high load/deflection ratio enable only limited activations so that any small change in activation will produce a very large change in the magnitude of the force released. In contrast, very flexible loops, i.e., with a very low load/deflection ratio, require a very large activation to produce the force magnitude for the desired retraction.12
T-loops, manufactured from 0.019 x 0.025-in stainless steel wire with a height of 7 mm and 10 mm horizontal dimension, deliver a force of about 250 g under a 1.5 mm activation. By reducing wire cross-section to 0.018 x 0.025-in or increasing the vertical height to 9 mm, or even using a TMA wire, the force released will be reduced when activated by 1.5 mm. The force will also vary in accordance with changes in the amount of activation, which can reach up to 3 mm without the risk of permanent loop deformation.11
During space closure, one should place in the molar region tip-back bends in the wire with an inclination of about 20° to 30° to control mesial tipping, while incorporating smooth bends of approximately 10° of lingual inclination in the third molars in order to prevent mesiolingual rotation.
It is advisable to have a panoramic radiograph taken after closing the spaces to assess root parallelism, especially in the area between second premolars and second molars. Should it become necessary to improve parallelism, second order bends (tip-backs) can be incorporated into the finishing archwires in the second molars. These teeth must remain tied together with metal ligatures to prevent the reopening of the spaces or to keep the omega loop tied back. The teeth should be kept together to allow a reorganization of the gingival fibers and bone maturation around the teeth, thereby reducing the possibility that the extraction spaces may reopened.
The use of Class II elastics increases the tendency of mandibular molars to tip mesially and incline lingually. Prolonged use of these elastics should therefore be avoided.
In first molar extraction cases, the interbracket distance between second molars and second premolars is considerable. In these areas one can observe wire deformation due to the chewing forces that are delivered to them. To avoid side effects in teeth adjacent to extraction spaces, these deformations need to be monitored frequently as they severely hinder sliding mechanics. If in this interbracket space the archwire is allowed to injure the soft tissues of the cheek, one can resort to plastic wire sheaths. The length of these sheaths should always be 1 to 2 mm smaller than the interbracket distance to prevent unwanted movements.
The use of archwires with loops allows the closure of first molar spaces with concurrent control of second and third molar mesial tip and lingual inclination. Control over inclination of posterior teeth in the buccolingual direction is obtained by incorporating torque.13
In its final stages, these auxiliaries must be repositioned so that the teeth can achieve their ideal position. The teeth adjacent to the extraction area that were banded in the early stages should have their attachments replaced by bonded brackets or tubes so that all spaces are fully closed with a fixed appliance.
Retention
The purpose of using posttreatment retention in all orthodontic cases is to prevent or reduce relapse. In adult patients, the main factors affecting posttreatment stability are the soft tissues surrounding the teeth, such as the tongue, perioral muscles, connective tissue of the periodontal ligament and gingival fibers.
Muscle function is a dominant factor in retention. If muscle balance is present, a well-established intercuspation may help to preserve the final tooth movement outcome. In cases with strong adverse muscle pressure, a precise relationship between the arches will not prevent the occurrence of relapse, requiring, therefore, a permanent retainer.
The lack of a reasonable occlusal balance during chewing can create instability. If the imbalance is excessive, future treatment may be necessary and/or occlusal adjustment should be performed to eliminate interference.
When a tooth is moved orthodontically, a fold or invagination of gingival tissue is formed between the teeth that were moved closer to each other. Apparently, these teeth are not moved through the gingiva, but rather compress the adjacent gingiva, producing an invagination of connective tissue and epithelium. The clinical appearance can vary from a single gap on the buccal side of the attached gingiva to a deep cleft that extends through the interdental papilla. The longer the time before initiating tooth movement after extraction, the greater the tendency of gingival invagination being formed.14,15
The invagination is considered as the main cause for the reopening of extraction spaces and it is therefore necessary to retain the teeth until reorganization of the pertinent structures has occurred. This remodeling may last 12 months in children and take even longer in adults.15
To reduce the possibility of relapse, Reitan16 recommends periodontal surgery before removing the fixed appliance. The surgery is aimed at cutting the elastic fibers located above the alveolar crest, which cause relapse. The orthodontic appliance should not be removed before recovery is complete.16
EXTRACTION OF PERMANENT SECOND MOLARS
Distal movement of maxillary first molars in cases of extraction of maxillary second molars occurs rapidly and efficiently, reducing treatment time and protrusion of anterior teeth, which is a common side effect when distalizing molars in cases without extractions.17,18
The space created by extracting second molars is usually larger than the space needed for correction of crowding and Class II. Nevertheless, anchorage must be considered, as there is significant mesial migration of molars during orthodontic treatment.17 With the advent of skeletal anchorage, concern about patient compliance in wearing headgear and intraoral elastics is no longer a determining factor in treatment success.
The main reasons to consider the extraction of second molars are: To prevent excessive profile flattening, which can occur with premolar extractions; to reduce treatment time, since one only uses the required amount of space to achieve an ideal molar occlusion relationship and a convenient first molar distalization.17,18 It also decreases the tendency of developing open bite in patients with an increased lower face.17,19
Second molar extraction is a viable alternative to be considered when these teeth are severely damaged or poorly positioned and when there is crowding in the posterior region, although it should not be considered as an alternative to replace premolar extraction in cases of dental crowding in the anterior region, or even in severe incisor protrusion cases.17,20,21
It is also indicated in cases of third molar impaction, despite the uncertainty involving its eruption in an acceptable position, and prevention of late crowding in the lower arch.17,18,20,21
One factor should be taken into account before recommending the extraction of second molars, i.e., verifying the presence of third molars, making sure they are well positioned and have an adequate coronary and root anatomy.17
The ideal time to recommend second molar extraction is when the third molars have begun root development, but it is not always possible to start orthodontic treatment in this phase, which does not preclude treatment in adults whose third molars have erupted.21
When treatment is started at the ideal stage it is usually completed before the eruption of third molars, causing, in some cases, extrusion of the opposing teeth (antagonists). Orthodontists must exercise caution and place an appropriate retainer. In cases where third molars erupt out of position and prevent the achievement of an adequate functional occlusion, orthodontic retreatment is indicated to position them correctly.21
In terms of relapses in the anteroposterior direction, cases treated with extraction of second molars seem to be quite stable.21
EXTRACTION OF PERMANENT THIRD MOLARS
General indications for removal of impacted third molars
The average age for eruption of third molars is around 20 years, although the eruption might continue as late as age 25.22
Third molars tend to tip distally during the early stages of development, and seldom tip mesially.23
Third molar begins to form horizontally tipped and eventually, with development and mandibular growth, the angulation changes from horizontal to mesioangular and ultimately to vertical.24
The ideal moment for extracting third molars is when more than 1/3 of the roots of these teeth have formed, usually between ages 17 and 20. The major issues related to retained third molars are addressed below.
Infections and inflammations
When a tooth is partially erupted and covered by the gingival operculum, the patient usually presents with repeated episodes of pericoronitis - an infection of the soft tissues around the crown of a partially erupted tooth - caused by normal oral microbiota. It is considered the most common disease related to impacted third molars. Third molars should not be extracted before the pericoronitis symptoms have been addressed.25
Root resorption
Root resorption of second permanent molars appears to be similar to the process of resorption that occurs with primary teeth in the presence of succeeding permanent teeth. After extraction of the impacted tooth, the adjacent tooth recovers through a cementum repair process. In a study on the prophylactic removal of asymptomatic third molars with a sample of 40 asymptomatic and impacted molars, 95% were referred for prophylactic removal with a 26% risk of root resorption of second molars.24,25
Odontogenic cysts and tumors
If the tooth is retained within the alveolar process, so is the dental follicle. This follicle, while maintaining its original size in most patients, can undergo cystic degeneration and become a dentigerous cyst or an odontogenic keratocyst. In general, if the follicle around the crown is larger than 3 mm, a dentigerous cyst should be suspected. Epithelial cells comprised within the dental follicle may also form an odontogenic tumor. Ameloblastoma25 is the most commonly found tumor in this region.
Inferior alveolar nerve impairment
The surgical removal of third molars may cause injury to the inferior alveolar nerve, which leads to a proliferation of axons, plausibly a cause of paresthesia, dysesthesia, allodynia and pain, which may eventually become disabling. However, inferior alveolar nerve injury is rare and other complications related to surgical removal of third molars such as pain and trismus should be considered.26
The pain following extraction of third molars is directly proportional to the degree of difficulty in extracting this tooth.27
General contraindications for removal of impacted third molars
In principle, all impacted teeth should be removed, except when there are specific contraindications. The most common contraindication for tooth extractions is age. An 18-year-old patient may present with swelling and discomfort for 1 or 2 days after the removal of an impacted tooth but a 50-year-old adult may display an edema for 4 to 5 days as a result of the same procedure. Therefore, patients older than 35 years with impacted teeth showing no signs of disease should not have these teeth extracted. Moreover, in patients over the age of 25, the risk of complications arising from the extraction of third molars increases.24
A very early extraction of third molars should be postponed until an accurate diagnosis of impaction can be established.24
Advanced age and compromised health are usually associated. In conditions involving compromised cardiorespiratory function (congenital or acquired coagulopathy), the surgeon is advised to leave the affected teeth in the alveolus until the general health of the patient is under control.24
Orthodontic indications for extraction of third molars
Currently, with the use of skeletal anchorage devices, it is possible to recommend the extraction of third molars with the purpose of creating space and correcting Class II by distalizing maxillary molars.28 A rate of 0.3 mm to 7.8 mm of distal movement of maxillary molars in a period of 7 months29 has been reported using this type of mechanics. Unlike other distalization mechanics, which provoke extrusion, it is possible to distalize upper and lower molars with intrusive vectors and with minimal risk of opening the bite.30
Orthodontic contraindications for extraction of third molars
Extraction of third molars is contraindicated in cases of extraction of permanent second molars as an alternative for the treatment of Class II. With the extraction of permanent second molars space is gained for distalization of first molars while the rest of the space is closed by moving the third molars mesially.22
CLINICAL CASE 1
Diagnosis summary
Forty-four-year-old patient presented as chief complaint mandibular crowding and space resulting from the extraction of tooth #26. On extraoral clinical examination she exhibited a pleasant looking face (Fig 1), lip competence, normal display of incisors on smiling, convex profile, normal nasolabial angle, nasal breathing, normal speech and swallowing.
Examination of the oral cavity revealed an Angle Class II Division 1, subdivision left molar relationship, less than 5 mm crowding, 50% overbite, 2 mm overjet, 2 mm lower midline deviation to the left and 1 mm upper midline deviation to the left, absence of tooth #26, tooth #43 positioned 3 mm mesially from tooth #33, and gingival recession in the cervical region of the canines, premolars and tooth #36 (Fig 1).
Periapical radiographic examination disclosed extensive restorations in posterior teeth with excess restorative material in the mesiodistal direction, and tooth #36 with lesions and furcation involvement (Fig 2). Cephalometric analysis revealed a skeletal Class II malocclusion, adequate inclination of the mandibular plane, incisors excessively inclined labially and a convex profile (Fig 3, Table 1).
Treatment goals
The goals were to align and level the teeth, establish intra-arch symmetry, close the extraction spaces, correct the deviated midlines, attain a normal second molar occlusion, establish adequate disocclusion guides and correct the overjet and overbite without changing the original facial esthetics.
Treatment planning
Treatment planning consisted in placing a standard Edgewise fixed orthodontic appliance, slot 0.022 x 0.028-in, on the upper and lower dental arches. The patient's teeth #16, #36 and #46 were extracted. During the alignment and leveling phase 0.012-in, 0.014-in and 0.016-in nickel-titanium wires were used, followed by 0.018-in stainless steel wire. While using 0.018-in wire, space closure was initiated with elastomeric chains to establish symmetry between the anteroposterior quadrants. Lower reverse curve of Spee was incorporated at this stage. Once symmetry was achieved, 0.019 x 0.025-in TMA wires with a T-loop were used to proceed with space closure.
When using the rectangular wires, a sharper curve of Spee was incorporated into the upper archwire for overbite control, as well as a tip-back bend placed in upper and lower molars to control the mesial tip. During the space closure phase, 5/16-in intermaxillary elastics with around 200 g of force on each side were used in the Class II direction to control anchorage and attain a normal molar occlusion. In the final stages upper and lower 0.019 x 0.025-in TMA archwires were used in coordination. A wraparound removable appliance was worn for retention in the upper arch 24h/day for 12 months. After this period, nighttime use was prescribed in order to prevent reopening the spaces created by the extracted molars. A 0.028-in steel wire was bonded to teeth #33 and #43 and a 0.020-in twist-flex wire was bonded to teeth #34, #35 and #37, #44, #45 and #47 to avoid reopening the spaces produced by the molar extractions.
Treatment results
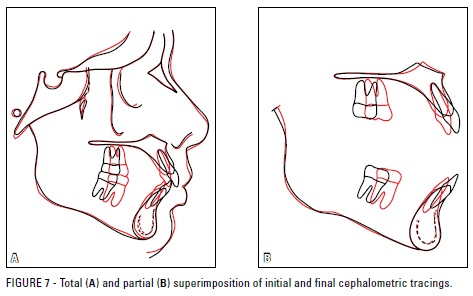
The treatment goals were achieved. The pleasant facial esthetics was preserved, second molars attained a normal occlusion, overjet and overbite were corrected in the anterior region and appropriate disocclusion guides were established. The upper incisors were uprighted, the lower incisors remained protruded, the teeth were aligned and leveled, the extraction spaces were closed and asymmetries corrected, the dental arch form was maintained (Fig 4) and the mandible experienced a counterclockwise rotation (Fig 7, Table 1).
From the beginning of treatment bone loss was apparent in the labial surface of tooth #36, which worsened after its removal. As a result, a periodontal defect developed in the mesial surface of tooth #37 (Fig 5). As regards case stability, the protracted use of an upper retainer became necessary, as well as the maintenance of a wire bonded to the teeth adjacent to the lower extractions.
CLINICAL CASE 2
Diagnosis summary
Female patient, age 23, presented as her chief complaint lip protrusion and the presence of posterior teeth with compromised crowns.
From a dental standpoint, as can be seen in Figure 8, she presented with an Angle Class I malocclusion, 10%, overbite, 2 mm overjet, coincident upper and lower midlines, severely damaged crowns of teeth #16, #26 and #47, which was confirmed by radiographic examination (Fig 9). The patient also featured parabolic arches with symmetry in the anteroposterior and transverse directions, negative 4 mm lower model discrepancy and absence of Bolton discrepancy. As regards her facial profile, she had a marked protrusion of both lips.
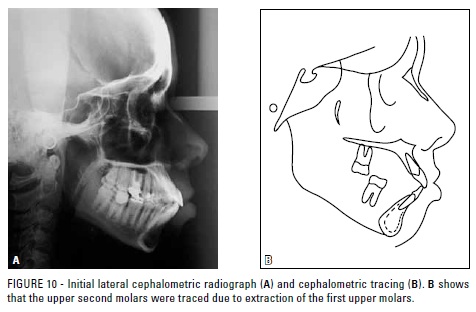
Assessment of a lateral cephalometric radiograph (Fig 10, Table 2) revealed an adequate inclination of the mandibular plane with incisors excessively inclined labially and a convex profile.
Treatment goals
To reduce the dental protrusion, establishing a correct incisor inclination and normal occlusion between the first lower molars and second upper molars.
Treatment method
Given that the patient rejected the placement of a skeletal anchorage device, it was explained that in order to reduce the dental protrusion and improve her profile convexity the treatment might require a second phase. In the first phase, teeth #16, #26, #37 and #47 would be extracted, the spaces closed, but the dental protrusion would likely only be fully corrected in a second phase, with the extraction of teeth #14, #24, #34 and #44.
A Nance button attached to the second molars was used for anchorage in conjunction with a Kloehn headgear and Class III elastics supported by the headgear to attain lower anchorage. The subject was referred for extraction of teeth #16, #26, #37 and #47 given the fact that the crowns were severely damaged. Archwire sequence and space closure were carried out as in Case 1, but with a different anchorage system.
After closing the molar spaces a new assessment was performed, where a slight retraction of the upper and lower incisors was noted as well as a minor change in her facial profile. The maxillary upper and lower first premolars were therefore extracted.
For retention, a removable (wraparound) retainer was used in the upper arch, and in the lower arch a twist-flex wire was bonded lingually from tooth #35 to tooth #45. The patient wore the retainer 24/7 during the first 12 months and, after this period, for nighttime use only.
Final results
In reviewing the patient's final records (Fig 11) it became clear that all intended goals were attained (Figs 5, 6 and 8). There was improvement in facial esthetics, a normal occlusion was achieved between maxillary second molars and mandibular first molars, appropriate overjet and overbite were achieved in the anterior region along with adequate disocclusion guides. The upper and lower incisors were uprighted (Fig 14, Table 2), the teeth were aligned and leveled, and the extraction spaces closed. A lateral cephalometric radiograph (Fig 13, Table 2) showed a reduction in tooth and lip protrusion.
Treatment lasted 51 months. A successful outcome was only possible thanks to patient motivation and youth, normal sized roots and the appropriate use of forces, which took into account the intervals between activations.
The root resorptions that the patient presented at the end of treatment (Fig 12) were acceptable given the movements performed, and entailed no periodontal involvement.
CLINICAL CASE 3
Diagnosis summary
Female patient, 33 years old, was referred by her dental implant surgeon to assess the possibility of closing the space of tooth #26, which was indicated for extraction. The patient had undergone previous orthodontic treatment with extraction of teeth #14 and #24. On extraoral clinical examination she exhibited a pleasant looking face, lip competence, normal display of incisors on smiling, convex profile and normal nasolabial angle (Fig 15).
Examination of the oral cavity revealed an Angle Class II malocclusion, absence of teeth #14, #24, #36, #46 and #47, 2 mm lower crowding, 15% overbite, 1 mm overjet, coincident lower midline and 1 mm upper midline deviation to the left (Fig 15). Periapical radiographic examination (Fig 16) disclosed that tooth #21 had undergone root canal therapy and tooth #26 had a perforation in the furcation area. Panoramic radiography displayed a divergence between the roots of teeth #13 and #15, and #23 and #25, and confirmed that teeth #14, #24, #36, #46 and #47 were missing (Fig 16). Cephalometric analysis (Fig 17, Table 3) revealed a skeletal Class I malocclusion, increased mandibular plane angle, incisors well positioned in their basal bone and a straight profile.
Treatment goals
The goals were to align and level the teeth, close the tooth extraction space created by tooth #26, upright tooth #48, correct the upper midline, establish appropriate disocclusion guides, correct overjet and overbite and preserve the original facial esthetics.
Treatment method
After placing the orthodontic appliance, the patient had tooth #26 extracted. A 0.018-in stainless steel wire was used to close the space by moving teeth #27 and #28 mesially. To this end, nickel-titanium springs were used with a force of approximately 200 g and on some occasions with elastomeric chains. For anchorage, a mini-implant was positioned between teeth #23 and #25. Figure 18 depicts the different stages of closing tooth #26 space. After space closure, panoramic and periapical radiographs were taken to evaluate root parallelism and integrity. In the finishing phase, upper and lower 0.019 x 0.025-in steel archwires were used in coordination. A wraparound removable appliance was prescribed for retention in the upper arch 24h/day for 12 months. After this period, nighttime use was indicated in order to prevent reopening of the spaces created by the extracted molar. In the lower arch, 0.028-in stainless steel wire was bonded from tooth #33 to tooth #43.
Treatment results
The treatment goals were achieved. The teeth were aligned and leveled, the space created due to the extraction of tooth #26 was closed, overjet and overbite were corrected in the anterior region, appropriate disocclusion guides were established, and facial esthetics was preserved (Fig 19). Panoramic radiography disclosed that tooth #48 was uprighted, the implant was positioned in the region of tooth #46 and the roots of teeth #25 and #27 were parallel to each other (Fig 20). Lateral cephalometric radiography showed that the facial profile was maintained (Fig 21). Cephalometric measurement evaluation showed no significant changes (Fig 22, Table 3). The only significant change consisted in the mesialization of the left upper second molar. Concerning case stability, the patient had to prolong the use of the upper retainer.
The use of a mini-implant in this case enabled unilateral space closure (tooth #26) and correction of the midline, which was already deviated to the side of the extraction. Sliding mechanics was not working efficiently with the use of 0.018 x 0.025-in wire and so the molars were mesialized with a 0.018-in wire. As a side effect, molar torque control was lost. The use of a mini-implant as indirect anchorage would allow the use of rectangular archwires with a space closure loop, enabling a more efficient torque control.
CLINICAL CASE 4
Male patient aged 50 years with a chief complaint of incisal wear and crowding.
On clinical extraoral examination, the patient featured a pleasant appearance, with lip competence and a concave profile (Fig 23).
Clinical intraoral examination revealed an Angle Class II, Division 2 malocclusion, with upper and lower crowding of 2 mm and 6 mm, respectively. The patient had a deep Curve of Spee, 20% overbite, 3 mm overjet, lower midline deviated 1 mm to the left side and a coincident upper midline. The upper and lower left side molars were in crossbite with the lower molars occluding buccally with the upper molars. The patient had a Bolton discrepancy of over 2 mm excess in the six anteroinferior teeth.
He did not have an adequate disocclusion guide on the left side due to premature contacts caused by the crossbite.
Panoramic and periapical radiographs revealed discreet horizontal bone loss, molar restorations and endodontic treatment in tooth #47 (Fig 24).
Cephalometric analysis showed a skeletal Class II, adequate inclination of the mandibular plane, protruded lower incisors and upright upper incisors (Fig 25, Table 4).
Treatment goals
The treatment was aimed at correcting the posterior crossbite, aligning and leveling the dental arches, correcting the Class II without changing facial esthetics and improving the disocclusion guides.
Treatment method
Extraction of the upper second molars was indicated with a view to correcting the Class II because the upper third molars had erupted with a normal anatomy. Furthermore, the lower third molar on the left side was missing and tooth #27 was involved in the crossbite. The upper first molars would be distalized with greater efficiency and only to the extent that it was necessary to ensure a correct intercuspation.
Alignment and leveling were performed by controlling lower incisor protrusion. To this end, a distributed 4 mm canine-to-canine stripping was performed in the lower arch in order to create space for the leveling of the curve of Spee, alignment of the 2 mm crowding that existed originally and elimination of the Bolton discrepancy.
After the complete alignment and leveling of the maxillary teeth, distalization of the first molars was initiated by means of a straight 0.018 x 0.025-in rectangular stainless steel wire and elastomeric chains both labially and palatally. The premolars and canines were also distalized with the binary system, until they reached a suitable position in relation to their antagonists. A Nance button supported by the third molars was used for anchorage.
After canine distalization, the Nance button was removed and space closure was completed with a slight movement of the maxillary incisors. At that time, the use of Class II intermaxillary elastics became necessary.
To correct the crossbite, starting with the use of a 0.018-in steel archwire, on the left side, the lower dental arch was subjected to contraction and the upper dental arch to expansion, both supported by the Nance button.
A wraparound-style upper retainer was indicated and a 0.028-in lingual canine-to-canine steel wire retainer was bonded to the lower arch.
At the end of the orthodontic treatment, the third molar on the right side was left with no antagonist and its extraction was indicated.
Treatment results
Esthetic appearance remained unchanged, the crossbite was corrected, the canine and molar relationship became a Class I malocclusion and the disocclusion guides were improved (Fig 26).
Bone level height in the molar region was maintained after space closure and treatment completion (Fig 27). There were no skeletal changes and there was control of lower incisor protrusion since these teeth were already protruding at the beginning of treatment (Fig 28, Table 4).
FINAL CONSIDERATIONS
The authors of this study contend that orthodontic treatment success in cases involving molar extractions is directly related to patient complaint and psychological profile, absence of disease and skeletal discrepancies, application of biomechanical principles and professional experience. Another factor worthy of consideration is whether the patient has undergone previous orthodontic treatment with extractions. These patients usually present with some degree of root resorption, a condition that can worsen, preventing such cases from being properly finished. Currently, skeletal anchorage allows the attainment of good results while reducing treatment time.
REFERENCES
- 1. Bennett JCM, McLauglin RP. O tratamento ortodôntico na dentição com aparelho pré-ajustado. São Paulo: Artes Médicas; 1998.
- 2. Sandler PJ, Atkinson R, Murray AM. For four sixes. Am J Orthod Dentofacial Orthop. 2000;117( 4):418-34.
- 3. Hom BM, Turley PK. The effects of space closure of the mandibular first molar area in adults. Am J Orthod. 1984;85(6):457-69.
- 4. Stepovich ML. A clinical study on closing edentulous spaces in the mandible. Angle Orthod. 1979;49(4):227-33.
- 5. Schroeder MA. Má oclusão Classe I de Angle com acentuada biprotrusão, tratada com extração de dentes permanentes. Dental Press J Orthod. 2009;14(4):137-48.
- 6. Carvalho RS, Nelson D, Kelderman H, Wise R. Guided bone regeneration to repair an osseous defect. Am J Orthod Dentofacial Orthop. 2003;123(4):455-67.
- 7. Feng X, Oba T, Oba Y, Moriyama K. An interdisciplinary approach for improved functional and esthetic results in a periodontally compromised adult patient. Angle Orthod. 2005;75(6):1061-70.
- 8. Kessler M. Interrelationships between orthodontics and periodontics. Am J Orthod Dentofacial Orthop. 1976;70(2):154-72.
- 9. Newman GV. Limited orthodontics for the older population: multidisciplinary modalities. Am J Orthod Dentofacial Orthop. 1992;101(3):281-85.
- 10. Roberts W, Chacker FM, Burstone CJ. A segmental approach to mandibular molar uprighting. Am J Orthod Dentofacial Orthop. 1982;81(3):177-84.
- 11. Braun S, Sjurse NRC, Legan H L. On the management of extraction sites. Am J Orthod Dentofacial Orthop. 1997;112(6):645-55.
- 12. Nanda R, Diaz MAT. Orthodontic space closure. Dent Clin North Am. 1981;25(1):95-107.
- 13. Stanley HR, Alattar M, Collett WK, Stringfellow HR Jr, Spiegel EH. Pathological sequelae of "neglected" impacted third molars. J Oral Pathol. 1988;17(3):113-7.
- 14. Diedrich P, Wehrbein H. Orthodontic retraction into recent and healed extraction sites. A histologic study. Am J Orthod Dentofacial Orthop. 1997;58(2):90-9.
- 15. Rivera Circuns AL, Tulloch JF. Gingival invagination in extraction sites of orthodontic patients: their incidence, effects on periodontal health, and orthodontic treatment. Am J Orthod Dentofacial Orthop. 1983;83(6):469-76.
- 16. Reitan K. Principles of retention and avoidance of posttreatment relapse. Am J Orthod. 1969;55(6):230-44.
- 17. Freitas MR, de Lima DV, de Freitas KM, Janson G, Henriques JF. Strategic maxillary second-molar extraction in Class II malocclusion. Am J Orthod Dentofacial Orthop. 2009;136(6):878-86.
- 18. Waters D, Harris EF. Cephalometric comparison of maxillary second molar extraction and nonextraction treatments in patients with Class II malocclusions. Am J Orthod Dentofacial Orthop. 2001;120(6):608-13.
- 19. Haas AJ. Let's take a rational look at permanent second molar extraction. Am J Orthod Dentofacial Orthop. 1986;90(5):361-3.
- 20. Richardson M, Mills K. Late lower arch crowding: the effect of second molar extraction. Am J Orthod Dentofacial Orthop. 1990;98(3):242-6.
- 21. Mezomo MB, Pierret M, Rosenbach G, Tavares CAE. A extração de segundos molares superiores para o tratamento da Classe II. Rev Dental Press Ortod Ortop Facial. 2004;15(3):94-105.
- 22. Moffit AH. Eruption and function of maxillary third molars after extraction of second molars. Angle Orthod. 1998;68(2):147-52.
- 23. Artun J, Behbehani F, Thalib L. Prediction of maxillary third molar impaction in adolescent orthodontic patients. Angle Orthod. 2005;75(6):904-11.
- 24. Peterson LJ, Ellis, Hupp EJR, Tucker MR. Princípios do tratamento de dentes impactados. In: Peterson LJ. Cirurgia oral e maxilofacial contemporânea. Rio de Janeiro: Elsevier; 2005. p. 197-205.
- 25. Almendros-Marqués N, Alaejos-Algarra E, Quinteros-Borgarello M, Berini-Aytés L, Gay-Escoda C. Factors influencing the prophylactic removal of asymptomatic impacted lower third molars. Int J Oral Maxillofac Surg. 2008;37(1):29-35.
- 26. Eriksson L, Hillerup S, Reibel J, Persson, Brun A. Traumatic changes of the inferior alveolar nerve and gasserian ganglion after removal of a mandibular third molar: report of a case. J Oral Maxillofac Surg. 2006;64(12):1821-5.
- 27. Lago-Méndez L, Diniz-Freitas M, Senra-Rivera C, Gude-Sampedro F, Gándara Rey JM, García-García A. Relationships between surgical difficulty and postoperative pain in lower third molar extractions. J Oral Maxillofac Surg. 2007;65(5):979-83.
- 28. Artese F. Pergunte a um expert. Rev Clín Ortod Dental Press. 2006;5(1)14-23.
- 29. Cornelis MA, De Clerck HJ. Maxillary molar distalization with miniplates assessed on digital models: a prospective clinical trial. Am J Orthod Dentofacial Orthop. 2007;132(3):373-7.
- 30. Sugawara J, Daimaruya T, Umemori M, Nagasaka H, Takahashi I, Kawamura H, et al. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 2004;125(2):130-8.
Molar extractions in orthodontics
Publication Dates
-
Publication in this collection
09 Mar 2012 -
Date of issue
Dec 2011
History
-
Received
31 May 2011 -
Accepted
10 Nov 2011