Abstract
The aim of this study is to report and analyze the effect of the More Doctors Program on the expansion of Family Medicine Residency (FMR), based on the strategies developed in Paraíba. A systematization of the experience was carried out by means of a conversation wheel, plus documentary analysis. A set of strategies (partnerships between Higher Education Institutions and Health Secretariats, state FMR workshops, institutional support of municipalities, articulation between the programs of provision of the federal government, regional residences, complementation of scholarship, among others) that resulted in new programs of FMR in interior of the state and a rate of expansion and occupation higher than the national average. This experience presented innovations and advances in the formation of generalists and in the teaching-service integration, with the consequent strengthening of Primary Care.
Keywords: Primary healthcare; More Doctors Program; Health personal management; Internship and residency
Resumo
O objetivo do estudo é relatar e analisar o efeito do Programa Mais Médicos (PMM) na expansão de programas de residência de Medicina de Família e Comunidade (RMFC), a partir das estratégias desenvolvidas na Paraíba. Realizou-se sistematização da experiência por meio de roda de conversa e análise documental. A partir da articulação dos atores locais integrada às políticas nacionais de expansão da RMFC, desenvolveram-se um conjunto de estratégias (parcerias entre instituições de ensino superior e secretarias de saúde, oficinas estaduais da RMFC, apoio institucional de municípios, articulação entre os programas de provimento do governo federal, residências regionais, complementação de bolsa, entre outros) que resultaram na interiorização da residência e em uma taxa de expansão e ocupação superior à média nacional. Essa experiência apresentou inovações e avanços na formação de generalistas e na integração ensino-serviço, com o consequente fortalecimento da Atenção Básica (AB).
Palavras-chave: Atenção primária à saúde; Programa Mais Médicos; Administração de recursos humanos em saúde; Internato e residência
Resumen
El objetivo del estudio es relatar y analizar el efecto del Programa Más Médicos en la expansión de programas de Residencia de Medicina de Familia y Comunidad (RMFC), a partir de las estrategias desarrolladas en el Estado de Paraíba. Se realizó la sistematización de la experiencia por medio de una ronda de conversaciones y análisis documental. A partir de la articulación de los actores locales, integrada a las políticas nacionales de expansión de la RMFC, se desarrolló un conjunto de estrategias (alianzas entre Instituciones de Enseñanza Superior y Secretarías de Salud, talleres estatales de la RMFC, apoyo institucional de municipios, articulación entre los programas de provisión del gobierno federal, residencias regionales, complementación de bolsa, entre otros) que resultaron en llevar la residencia al interior del estado y en un índice de expansión y ocupación superior al promedio nacional. Esta experiencia presentó innovaciones y avances en la formación de generalistas y en la integración enseñanza-servicio, con el consiguiente fortalecimiento de la Atención Básica.
Palabras-clave: Atención primaria de la salud; Programa Más Médicos; Administración de recursos humanos en salud; Internado y residencia
Introduction
Brazil has been adopting a care model based on care networks orchestrated by primary care in a perspective that is similar to other countries1. Over the last few years, some measures, such as the implementation and expansion of the Family Health Strategy (ESF), increase of funds, and assessment and induction mechanisms to improve quality, were implemented. As a result, the care coverage was expanded, ensuring an improvement in health indicators2.
Despite these results, weaknesses in the access to the Brazilian primary care and in its quality are observed, particularly its poor capability of solving problems. Regarding access, the deficit in the number of doctors, particularly in places with the worst human development indices, was one of the things that limited the expansion of primary care, being, therefore, opposed to the principle of equity3. Another relevant aspect is the small number of doctors with the characteristics and qualification to work in primary care: family and community doctors represent approximately 1.2% of Brazilian doctors and 5% of doctors who work in primary care4.
Over the last decades, the Brazilian Ministry of Health and the Ministry of Education implemented initiatives to foster the education of general practitioners and expand educational activities in primary care. Among these initiatives, the following are highlighted: Program of Education through Work for the Area of Health (PET-Saúde), National Support Program to the Education of Specialist Doctors in Strategic Areas (Pró-Residência) and Qualification Program for Primary Care Professionals (PROVAB)5.
Pró-Residência was created in 2009. It was aimed at supporting the education of specialists in deprived regions and priority specialties to SUS6. This program had a great impact on the creation of seats and reduction of regional inequalities in the distribution of residency seats6.
PROVAB was created by the Ministry of Health in 2012. It was aimed at encouraging health professionals to work in ESF. In order to do that, the Ministry of Health offered study-work scholarships and pedagogical support through distance specialization and in-person supervision7. Additionally, the program offered a 10% bonus on the grade of the residency selection test. This was its most criticized element, since it goes against a meritocratic concept. However, both programs had a limited impact on the search for a Family and Community Medicine (FCM) education7.
Concern about the gap between the number of family health teams (around 34,000 in 2013) and the existence of only 3,250 FCM in the country8 showed disparity between social needs and the educational ability of specialists. Regarding future needs, by assessing the occupancy rate and the number of residency seats in 2012, it is observed that the annual rate of education of new family doctors would be lower than 300 per year. This number was insufficient to meet the needs provided for in the National Health Plan (2012-2015). The plan forecasted an annual expansion of 1,325 new family health teams9.
Based on the More Doctors Program (PMM), initiatives were implemented in medical education, directly impacting Family and Community Medicine Residency (FCMR) programs. Law 12871/2013, which created the program, aims at universalizing access to medical residency and requiring one to two years of FCMR as a prerequisite to be inserted in most of the other residency programs3,10.
In this sense, strategies to strengthen preceptorship and incite integration between undergraduate courses and FCMR were determined, encouraging the participation of medical schools in the residency expansion process. In order to strengthen preceptorship, the creation of the National Preceptor Education Plan to the FCMR programs is highlighted. It enabled a specific funding to preceptorship11. Regarding the induction of integration between undergraduate courses and residency, several normative instruments related to the authorization and assessment process of medical schools led to new FCMR seats and other priority specialties. Therefore, all schools were encouraged to accredit new FCMR programs or expand seats in the existing ones.
These rules also determined that new private medical schools should create, throughout its first six years of operation, a number of FCMR seats equivalent to the number of admission seats in the course authorization process12. This association was aimed at ensuring the residency programs’ quality and instigating the interiorization and medical retainment process. Studies show medical retainment is potentialized when both the undergraduate course and residency are taken in the same region13,14.
The suggested legal changes and the role assigned to FCMR in the new scenario resulted in the need to reorganize FCMR programs, determine the scope of medical specialty and of the competencies expected from family doctors15 taking into consideration the Brazilian primary care reality. Strengthening the resident’s role as part of the ESF team was also important. This was made possible through the Ministry of Health’s 2012 directives with a new boost to reorganize this education focused on work16.
After four years of implementation of this program, it is essential to analyze this initiative and its future perspectives in a context of investment cuts in the health sector, especially in primary care. Therefore, this study aims at reporting and analyzing PMM’s effects in the expansion of FCMR based on experiences in the Brazilian state of Paraíba.
Methodology
This study was a systematization of experiences17 in which agents/researchers analyzed their own practice. The residency expansion process in FCM was analyzed based on experiences of teachers/researchers of the Health Promotion Department of Universidade Federal da Paraíba (UFPB). The teachers/researchers are directly implied in the education of the state’s doctors and develop activities connected to PROVAB, PMM, FCMR and undergraduate medical courses.
Qualitative and quantitative methodological approaches were used in this systematization. A conversation circle was held with nine teachers/researchers to discuss/analyze experiences. The circle did not have a structured script and was collectively mediated by its participants. The participants freely discussed their experiences collectively producing an analysis18. The circle was recorded in real time based on individual notes, which were consolidated into a collective report. This report was provided in an asynchronous virtual communication tool where the agents kept their conversation. All narratives were analyzed based on the identification of sense nuclei produced by the agents. The nuclei structured the analysis lines and determined this article’s sections19.
A documentation analysis was also conducted in the reports of the activities developed by the agents under the scope of PROVAB, PMM, federal government’s directives published from 2012 to 2017 related to medical education, and documents related to FCMR published from 2010 and 2017. The reports were provided by Paraíba’s Program Coordination. The directives were accessed on the Ministry of Health’s webpage. An exploratory and analytical qualitative study was conducted on these documents20. After determining the material, an exploratory reading was conducted, followed by selective, analytical and interpretative readings. The first reading aimed at selecting material related to the research’s questions. The subsequent readings aimed at building syntheses to help understand the study’s object21.
In the quantitative approach, data collected from secondary databases related to the 2010-2017 period was analyzed. The number of residency seats in the country was obtained from data from the National Medical Residency Committee (CNRM), provided by the Brazilian Society of Family and Community Medicine (SBMFC). Information related to Paraíba was collected through excerpts from CNRM’s authorization acts and information provided by Medical Residency Committees (COREME).
All accredited seats for first-year residents were taken into consideration in the analysis. Data related to seat occupancy and FCMR’s organization model was directly collected from the programs’ supervisors and COREME. National data was provided by SBMFC. Seats taken by the end of the first residency month were considered occupied.
Data related to the number of ESF teams was obtained from the Ministry of Health’s Primary Care Department portal. Data related to PROVAB and residency operation was collected from the program’s reports recorded by the local coordination from 2012 to 2017. Records were tabulated and went through a descriptive stage that enabled to obtain absolute and relative data. This data was presented on tables, graphs and figures, which enabled to understand quantitative aspects related to the distribution of residency seats in the state.
Results
The FCMR expansion process in Paraíba had some peculiarities. It was seen as an opportunity to qualify the state’s primary care and transform it into an environment of education of specialized doctors. Consequently, FCMR acquired a truncal characteristic22. This understanding of some involved agents is explained by the fact that, in 2014, approximately one third of the state’s team depended on PMM’s supply axis to keep doctors in Primary Care Units (UBS). Due to this fact and to the time limit in the supply of doctors through PMM, Paraíba would need to be prepared to equip its network with qualified doctors to primary care at the end of the program. In order to achieve this objective, a group of agents was based on national policies, such as Pró-Residência, and rules to induce changes in order to integrate undergraduate courses with FCMR programs and build a state medical education process focused on primary care.
Initially, the goal was to gradually replace PROVAB seats with FCMR program seats. In a context of primary care qualification, including its organizational role22, it would be possible to further believe in FCMR undertaking a decisive role in the consolidation of SUS. In Table 1, these actions were successful, and currently more than 10% of the state’s ESF teams are connected to FCMR.
Evolution in the number and percentage of ESF teams with doctors connected to PROVAB and Family and Community Medicine Residency Programs, 2012 to 2017, Paraíba.
Paraíba’s uniqueness can be explained by a series of agreements for the construction of a local network articulating different agents and institutions. Therefore, the residency expansion process in Paraíba was characterized by a large integration between education institutions and health departments, interiorization of residency seats, dialog among different residencies in the state, operation of different PROVAB/PMM agents and permanent management awareness through their representative institutions. Some actions will be reported below, and some of the achieved results will be presented, compared with national seat occupancy data.
Expansion process in Paraíba: new agents and meetings to create an education network
With PMM, new agents started operating in a structured way to apply and consolidate the program through its State Coordination Commission (CCE). In its minimum composition, CCE is comprised of representatives of the Ministry of Health, State Department of Health (SES), Council of Municipal Health Secretaries (COSEMS) and supervising institutions that used to be federal higher education institutions in Paraíba23. In Paraíba, CCE also had representatives of the Ministry of Education, since it was considered a relevant agent in a cross-sectional policy where the educational axis is one of PMM’s structuring axes.
In 2015, CCE started playing an essential role in the discussion of FCMR expansion and interiorization. Among its attributions, it is aimed at guiding its works towards the National Primary Care Policy, promoting articulation with the Permanent Teaching-Service Integration Commission and promoting Permanent Health Education Forums23. This clarifies its articulating characteristic in the debate related to primary care qualification and teaching-service integration.
Understanding its potential to articulate different institutions interested in qualifying primary care in Paraíba, CCE started the debate among agents. Several fronts of action were created in order to raise awareness of city managers and higher education institutions to adhere, qualify and expand residency to improve occupancy of idle FCMR seats.
In this context, Paraíba’s CCE used some devices: 1. articulation with SES to discuss FCMR’s path in the state; 2. presentation of medical residency to COSEMS; 3. participation in meetings of Regional Intermanagerial Commissions (CIR); 4. state workshops to foster the debate on the educational axis with managers and higher education institutions; 5. diagnosis of the necessary services network to implement FCMR; 6. taking advantage of the matrix-based structure of PROVAB cities; 7. meeting with PROVAB and PMM supervisors and tutors to discuss residency and the supervisor’s role in this process; and 8. permanent dialog with the Ministry of Health’s decentralized references, acknowledgement and approximation of these agents with city managements since the creation of the program. The main actions to better understand the process and its relevance to the articulation of network processes are detailed below.
Articulation between higher education institutions and SUS managers: combining network points
In order to build a process with local political legitimacy, CCE promoted dialog spaces with different local managers and higher education institutions. An important characteristic of these spaces was the fact that they were promoted in partnership with SES and COSEMS. Events aimed at discussing the educational axis were held, presenting FCMR as the main strategy in the primary care qualification process. The following was articulated for these dialogs: PROVAB’s coordination, PMM’s tutors, supervisors from both programs, decentralized references from the Ministry of Health and the Ministry of Education, CCE’s members, managers, medical course coordinators, health secretaries, SES, CIR/PB and COSEMS’ presidents, COREME’s representative, FCMR’s coordinators and the State Educational Center.
Three workshops were held. Based on them, CCE was able to discuss the construction and consolidation of municipal residencies, pedagogical models, primary care qualification strategies and professional retainment strategies based on residency.
These workshops provided an exchange of experiences among several FCMR programs in the state. Difficulties, often similar ones, positive initiatives and joint perspectives of health network qualification and integration among programs were shared. Important strategies to be implemented in the state were also articulated with COSEMS. An examples of these strategies was the creation of municipal incentives and laws to support the resident scholarship complementation, payment of preceptors, and teaching-service integration experiences, involving undergraduate courses and residency.
These meetings enabled to identify and recognize agents, which was essential to build the idea of belonging to a state FCMR education network. As a result, an action plan was created, which included: 1. permanent integration between state residencies and SUS managers based on the Education-Health Public Action Organizational Contract (COAPES); 2. creation of a debate agenda in CIR and Bipartite Intermanagerial Commissions (CIB) so that the cities could familiarize and take part in the creation of residencies; 3. creation of strategies of higher education institutions and cities that already have residency in order to expand seats and increase occupancy of idle seats; 4. PROVAB’s support to residencies that were weak and could not fill their seats.
Diagnosis of the necessary services network to implement FCMR
SES and the Ministry of Health’s primary care coordination surveyed the state’s health networks. CCE classified Paraíba’s 223 cities into their “potential for regional residency,” “potential for municipal residency,” “potential for residency expansion or qualification” and “non-priority city,” according to their priority to discuss residency in six months. In this diagnosis, the following was taken into account: history of the city’s participation in the program, ability to welcome residents in mandatory internships for a residency to be approved, network’s structure, primary care organization process, existence of professionals with preceptorship profile, ability to articulate among the region’s cities, existence of undergraduate courses or being fields of practice in health. This process enabled to identify the cities and regions with potential for teaching-service integration activities, as recommended by the National Policy for Permanent Health Education (PNEPS)24.
Subsequently, for one year, CCE members attended meetings involving 76 cities with potential for having regional or municipal residency. Additionally, the representative of Patos’ regional residency (which began in 2016 with the challenge of allocating 36 residents in the state’s small towns) articulated cities of four health microregions for an agreement of fields of residency. Both movements contributed to the cities’ familiarity with FCMR proposal and unchaining a pioneer process in the state of FCMR interiorization in places where there are no medical education institutions.
Institutional support to cities
Despite the initiatives unleashed by CCE in the state level and even though the regulatory devices were essential, a significant part of the strategies are constituted of mechanisms that induce changes and are developed in a context of autonomy of local agents. Having this in mind, an institutional support process was established to priority cities. It was based on the idea of support as a work management device based on the shared production of knowledge25. The proposal was to visit the cities in order to identify their potentialities and difficulties, and build with them strategies to strengthen the FCMR education network.
In order to do so, PROVAB’s supervisors, along with the Ministry of Health’s decentralized references who already had previous knowledge of the region, initially paid monthly visits to these strategic cities. Since it was a result of the agents’ meeting, the support was conducted in different forms, depending on the city and/or region. Therefore, the agents attended CIR meetings and paid visits to health units that could hold residency. Additionally, project proposals/models of regional FCMR programs, and rules and proceedings to claim a residency program or partner with existing programs were presented. The cities that decided to create their own program were provided with support throughout the pedagogical project organization and request submission to CNRM. The pedagogical projects were created based on meetings between different managers and PROVAB’s supervisors. Their perspective was to work as a device to structure the education of professionals to primary care and strengthen regional care networks.
This process involved 6, from the 16, health microregions of Paraíba, with 100 cities. It directly supported a plea of a program in the second microregion, with four seats, and the involvement of two other microregions as fields of internship.
The first looks on the state repercussions of the national and local process to induce changes
In this entire process, the FCMR construction in Paraíba differentiates from the national one in the high occupancy rate and in the important increase of cities offering residency seats, which characterized the FCMR interiorization process in the state. In 2010, only two cities offered residency seats, but with occupancy difficulties. In 2017, residents were redistributed into the four macroregions, in the state’s 24 cities (Figure 1). This shows an interiorization process of residency, as encouraged by the national policy.
Besides the interiorization, the encouragement of small, medium and large cities to participate in the doctors’ educational process was innovative. Based on this encouragement, FCMR was included in CIR’s discussions; some cities opened up for being fields of internship of other programs, strengthening the higher education institutions’ partnership with municipal health departments; a health region sent a project that was approved; and several cities became aware of building regional projects.
On the other hand, institutional relationships were qualified where there already was FCMR. These partnerships between higher education institutions and municipal health departments resulted in: creation of management boards, increase in the capability to solve problems; expansion of the scope of primary care practices; recruitment of preceptors; and payment of scholarship complementation to residents. Due to the territory’s diversity, contracts were different: in some residencies, preceptors were hired by the city for 40 hours as primary care doctors and were responsible for 2 to 4 residents; in others, they were hired by the higher education institution itself. The resident’s scholarship complementation was conducted in three ways: the city paid the scholarship through a municipal directive; as a service provision; or they were primary care doctors who passed examinations, already had a statutory bond, worked in residency in the UBS and had a salary in addition to the Ministry of Health’s scholarship. Several cities are discussing and drafting scholarship complementation laws for residents and preceptors.
Another relevant aspect was the perception of the positive impact of these actions in the qualification of teaching in undergraduate courses due to the expansion of possibilities of preceptorship and of scenarios of practice in primary care, both in the first years of the course and in internship, since the top-ranked units were those where interns followed residents. Considering this teaching-service integration that qualify both, one of the medical courses in Paraíba’s backcountry created a regional residency with 36 annual seats involving different cities. They believed that, in order to have a qualified course, they first needed to qualify the services network.
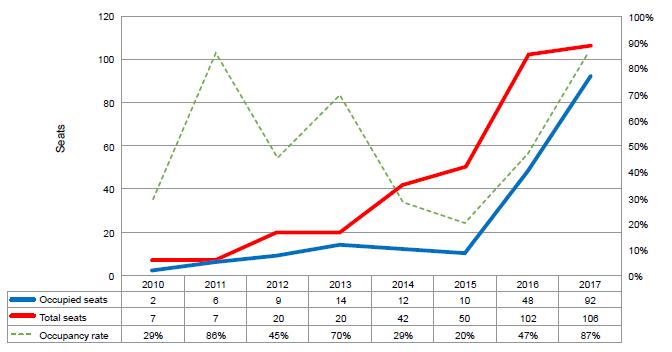
Lastly, analyzing in a more quantitative way the general result of the state’s interventions, Graph 1 shows a large expansion of FCMR seats, with an increase of more than ten times from 2010 to 2017. Currently, the programs’ occupancy rate is 87% - 2.5 times more than the national rate. The occupancy rate varied throughout the period. It presented a downward trend from 2013 to 2015, when the process was reversed, returning to its previous levels at the same time that national strategies of seat occupancy were strengthened and state strategies to transform Paraíba’s primary care into an educational center were conducted. In the national level, as shows Graph 2, from 2010 to 2017, there was an increase of 4.5 times in the number of seats, with a low seat occupancy rate of only 35%. This shows a chronic problem, despite the national measures to induce changes. When comparing national and Paraíba’s data, a greater effectiveness is observed in the residency expansion and occupancy process. This development is related to teaching-service integration mechanisms and to the synergic work of SUS managers and higher education institutions, generating unique movements, as established by PNEPS.
Evolution in the total number of seats and occupied seats in FCMR programs and occupancy rate; 2010 to 2017, Paraíba.
Evolution in the total number of seats and occupied seats in FCMR programs and occupancy rate; 2002 to 2017, Brazil.
Final remarks
The FCMR expansion and occupancy process in Paraíba has positive results that are better than the national average. With a synergic local and regional operation, the combination of federal policies of work and health education management, and of primary care expansion provided a series of innovations aimed at strengthening the teaching-service integration and the construction of shared spaces of planning and management between education institutions and local SUS managers.
In summary, a policy that, in several places, was restricted to supplying doctors, in Paraíba, it was consolidated as a strategy to induce changes in the education of professionals, articulating several SUS agents in the construction of this education and care network according to the needs of Paraíba’s population.
Additionally, the development of regional residency programs and their CIR-based organization evidence the great potential of the teaching-service integration to strengthen the regionalization and SUS process. They also indicate the possibility of city managers becoming protagonists in building a network of education of FCM specialists. This can be essential in a continental country comprised of small and medium cities that generally have different needs from larger cities.
Another important point is that municipal initiatives to foster preceptorship and complement scholarships can improve occupancy rates in the programs. However, it is also important to consider professional retainment devices after the residency’s conclusion. In Paraíba, the complementation of scholarships did not involve the third sector and exclusively involves the city. This fact could be discussed in order to create municipal laws to consolidate this policy.
The application of these strategies, especially at the regulatory level, can equate Brazil to other countries where the proportion of FCM seats corresponds to more than 30% of the country’s residency seats. Additionally, in the long term, it could also supply qualified doctors to work in primary care.
On the other hand, the intense debate that started with PMM’s creation shows that, in order to play its role as organizer of the education of workers, the state also needs to discuss concepts that are already instituted in the current society, such as merit. The logic of commitment and social responsibility with the Brazilian population and consequently with SUS consolidation should be added to the concept. Additionally, it is necessary to resignify the role of managers of SUS and higher education institutions and to establish new management and dialog mechanisms among all agents involved in medical education.
References
- 1 Giovanella L, Mendonça MHM, Almeida PF, Escorel S, Senna MCM, Fausto MCR, et al. Family health: limits and possibilities for an integral primary care approach to health care in Brazil. Cienc Saude Colet. 2009; 14(3):783-94.
- 2 Costa JSD, Teixeira AMFB, Moraes M, Boing AF, Strauch ES, Silveira DS, et al. Redução das internações por condições sensíveis à Atenção Primária no Brasil entre 1998-2009. Rev Saude Publica. 2012; 46(2):359-66.
- 3 Brasil. Ministério da Saúde. Secretaria de Gestão do Trabalho e da Educação na Saúde. Programa mais médicos - dois anos: mais saúde para os brasileiros. Brasília: Ministério da Saúde; 2015.
- 4 Pérez PB, López-Valcárcel BG, Vega RS. Oferta, demanda y necessidad de médicos especialistas em Brasil: proyecciones a 2020; 2011. Rio de Janeiro: Sociedade Brasileira de Medicina de Família e Comunidade; 2012.
- 5 Dias HSA, Lima LD, Teixeira M. A trajetória da política nacional de reorientação da formação profissional em saúde no SUS. Cienc Saude Colet. 2013; 18(6):1613-24.
- 6 Alessio MM, Sousa MF. Regulação da formação de especialistas: inter-relações com o Programa Mais Médicos. Physis. 2016; 26(2):633-67.
- 7 Carvalho MS, Sousa MF. Como o Brasil tem enfrentado o tema provimento de médicos? Interface (Botucatu). 2013; 17(47):913-26.
- 8 Scheffer M, Cassenote A, Biancarelli A. Demografia médica no Brasil: cenários e indicadores de distribuição. São Paulo: Conselho Federal de Medicina; 2013.
- 9 Brasil. Ministério da Saúde. Plano Nacional de Saúde - PNS: 2012-2015. Brasília: Ministério da Saúde; 2011.
- 10 Brasil. Presidência da República. Lei nº 12.871, de 22 de Outubro de 2013. Institui o Programa Mais Médicos. Diário Oficial da União. 23 Out 2013.
- 11 Brasil. Ministério da Saúde, Ministério da Educação. Portaria Interministerial nº 1.618, de 30 de Setembro de 2015. Institui, o Plano Nacional de Formação de Preceptores para os Programas de Residência na modalidade Medicina Geral de Família e Comunidade nos termos da Lei nº 12.871, de 22 de outubro de 2013. Brasília. Ministério da Saúde, Ministério da Educação; 2013.
- 12 Brasil. Secretaria de Regulação do Ensino Superior, Ministério da Educação. Edital nº 6/2014/SERES/MEC. Edital de seleção de propostas para autorização de funcionamento de cursos de medicina em municípios selecionados no âmbito do edital nº 03, de 22 de outubro de 2013. Diário Oficial da União. 23 dez 2014.
- 13 Seixas PHDA, Correa AN, Moraes JC. Migramed - Migração médica no Brasil: tendências e motivações. São Paulo: Observatório de Recursos Humanos em Saúde de São Paulo; 2014.
- 14 Adler B, Biggs WS, Bazemore AW. State patters in medical scholl expansion, 2000-2010: variation, discord and policy priorities. Acad Med. 2013; 88:1849-54.
- 15 Brasil. Comissão Nacional de Residência Médica. Resolução CNRM nº 1/2015. Regulamenta os requisitos mínimos do Programa de Residência Médica em Medicina Geral de Família e Comunidade - R1 e R2 e dá outras providências. Brasília: Ministério da Educação; 2015.
- 16 Brasil. Ministério da Saúde. Portaria nº 3.147, de 28 de Dezembro de 2012. Institui as especificações "preceptor" e "residente" no cadastro do médico que atua em qualquer uma das Equipes de Saúde da Família previstas na Política Nacional de Atenção Básica. Brasília: Ministério da Saúde; 2012.
- 17 Holliday OJ. Dilemas y desafíos de la sistematización de experiencias. In: Seminario ASOCAM; 2001; Cochabamba. Cochabamba: Intercooperation; 2001.
- 18 Bernardes JS, Santos RAS, Silva LB. A Roda de Conversa como dispositivo ético-político na pesquisa social. In: Lang CE, Bernardes JS, Ribeiro MAT, Zanotti SV, organizadores. Metodologias: pesquisas em saúde, clínica e práticas psicológicas. Maceió: EDUFAL; 2015. p. 13-34.
- 19 Spink MJ. Práticas discursivas e produção de sentidos no cotidiano: aproximações teóricas e metodológicas. São Paulo: Cortez; 2000.
- 20 Gil AC. Métodos e técnicas de pesquisa social. São Paulo: Atlas; 1999.
- 21 Gil AC. Como elaborar projetos de pesquisa. São Paulo: Atlas; 2002.
- 22 Magalhães Junior HM, Pinto HA. Atenção básica enquanto ordenadora da rede e coordenadora do cuidado: ainda uma utopia? Divulg Saude Debate. 2014; 51:14-29.
- 23 Brasil. Ministério da Saúde. Portaria nº 2.921, de 28 de Novembro de 2013. Dispõe sobre a constituição das Comissões Estaduais e Distrital do Projeto Mais Médicos para o Brasil. Brasília: Ministério da Saúde; 2013.
- 24 Brasil. Ministério da Saúde. Política Nacional de Educação Permanente em Saúde. Brasília: Ministério da Saúde; 2009.
- 25 Campos GWS, Domitti AC. Apoio matricial e equipe de referência: uma metodologia para gestão do trabalho interdisciplinar em saúde. Cad Saude Publica. 2007; 23(2):399-407.
Publication Dates
-
Publication in this collection
20 May 2019 -
Date of issue
2019
History
-
Received
20 Jan 2018 -
Accepted
08 Oct 2018

 The More Doctors Program and Family and Community Medicine residencies: articulated strategies of expansion and interiorization of medical education
The More Doctors Program and Family and Community Medicine residencies: articulated strategies of expansion and interiorization of medical education