We report the case of a 74-year-old male patient with a one-year history of chest pain in the suprasternal notch associated with erythema, edema and drainage of purulent material from a fistulous lesion. The patient was HIV-negative with no history of TB. A CT scan of the chest showed an osteolytic lesion in the sternum, and a biopsy revealed caseous granuloma, which, in the microbiological evaluation, was negative for fungi and acid-fast bacilli. The diagnosis of sternal osteomyelitis caused by Mycobacterium tuberculosis was confirmed using PCR.
Descrevemos o caso de um paciente de 74 anos, masculino, com dor torácica na porção superior do esterno com um ano de evolução associada a eritema, edema e fístula com drenagem de material purulento. Paciente HIV negativo e sem história prévia de contato com TB. A TC de tórax evidenciou lesão osteolítica esternal, e o material de biópsia revelou granuloma caseoso negativo para fungos e bacilos álcool-ácido resistentes no exame microbiológico direto. O diagnóstico de osteomielite esternal por Mycobacterium tuberculosis foi realizado por PCR.
Tórax; Infecções por Mycobacterium; Tuberculose osteoarticular; Esterno; Diagnóstico
CASE REPORT
Sternal osteomyelitis caused by infection with Mycobacterium tuberculosis*
Diego Michelon De CarliI; Mateus Dornelles SeveroII; Carlos Jesus Pereira HaygertIII; Marcelo GuolloIV; Alex OmairiV; Vinícius Dallagasperina PedroVI; Eduardo Pedrolo SilvaVI; Arnaldo Teixeira RodriguesVII
IResident in Gastroenterology. São Vicente de Paulo Hospital, Passo Fundo, Brazil
IIResident in Clinical Medicine. Santa Maria University Hospital, Federal University of Santa Maria, Santa Maria, Brazil
IIIAssistant Professor of Radiology. Santa Maria University Hospital, Federal University of Santa Maria, Santa Maria, Brazil
IVResident in General Surgery. Santa Maria University Hospital, Federal University of Santa Maria, Santa Maria, Brazil
VResident in Cardiology. Institute of Cardiology, University Cardiology Foundation, Porto Alegre, Brazil
VIMedical Student. Federal University of Santa Maria School of Medicine, Santa Maria, Brazil
VIIAssistant Professor of Clinical Medicine. Santa Maria University Hospital, Federal University of Santa Maria, Santa Maria, Brazil
Correspondence to
ABSTRACT
We report the case of a 74-year-old male patient with a one-year history of chest pain in the suprasternal notch associated with erythema, edema and drainage of purulent material from a fistulous lesion. The patient was HIV-negative with no history of TB. A CT scan of the chest showed an osteolytic lesion in the sternum, and a biopsy revealed caseous granuloma, which, in the microbiological evaluation, was negative for fungi and acid-fast bacilli. The diagnosis of sternal osteomyelitis caused by Mycobacterium tuberculosis was confirmed using PCR.
Keywords: Thorax; Mycobacterium infections; Tuberculosis, osteoarticular; Sternum; Diagnosis.
Introduction
The extrapulmonary form of TB involving the sternum is quite rare. The most significant risk factor for the disease is open heart surgery.(1) Other risk factors include intravenous drug abuse, blunt thoracic trauma, closed cardiopulmonary resuscitation, subclavian vein catheterization, diabetes mellitus, HIV infection, alcoholism and BCG vaccination.(1) Sternal TB usually affects young adults living in areas where TB is endemic. Since the advent of modern antituberculous therapy, the number of cases of sternal TB has dramatically decreased, there having been fewer than 20 cases reported in the literature since that time.(2) We report the case of a male patient without active pulmonary disease who was under follow-up treatment at a clinical medicine outpatient clinic when he developed sternal TB.
Case report
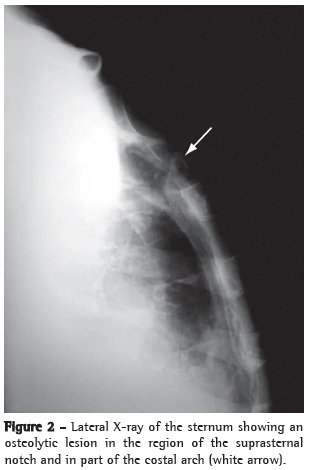
A 74-year-old white male who was a retired farmer, a nonsmoker and a former drinker presented with a one-year history of chest pain in the suprasternal notch, accompanied by edema and local erythema. His condition had worsened two weeks prior, aggravated by drainage of purulent material from a fistulous lesion. In addition, he reported evening fever, night sweats and weight loss (25 kg) in the last 12 months. The patient was under outpatient follow-up treatment in various sectors of the Santa Maria University Hospital, due to multiple comorbidities: systemic arterial hypertension; heart failure; mitral valve disease; pulmonary arterial hypertension; hypothyroidism; chronic renal failure; nonspecific colitis; and benign prostatic hyperplasia. He was being treated with furosemide, simvastatin, omeprazole, levothyroxine, hydralazine, clonazepam, sertraline, finasteride and doxazosin. Physical examination at admission revealed satisfactory general heath, extremely pale mucosae, an arterial pressure of 130/80 mmHg, a heart rate of 80 bpm, an axillary temperature of 36ºC and a respiratory rate of 35 breaths/min. The patient presented a grade 3/6 systolic ejection murmur at the apex, radiating to the axillary region, and diminished breath sounds at both lung bases. In the region of the suprasternal notch, there was a poorly delineated, hyperemic edematous area (approximately 10 cm in diameter) that was painful upon palpation and presented drainage of purulent secretion from a fistulous lesion (Figure 1). A swab specimen of the lesion was collected, and an open sternum biopsy was performed for histopathological analysis. Treatment with ciprofloxacin and clindamycin was initiated. The blood workup revealed normochromic normocytic anemia, the PPD test was positive (induration = 15 mm), HIV testing (ELISA) was negative, and erythrocyte sedimentation rate (ESR) was 48 mm/h. Imaging studies (anterior and lateral chest X-rays) revealed no pleuropulmonary findings suggestive of previous or active TB. A lateral X-ray of the sternum revealed an osteolytic lesion in the region of the suprasternal notch and the first costal arches (Figure 2). A CT scan of the chest revealed an osteolytic lesion in the suprasternal notch, without mediastinal invasion, as well as bilateral transudative pleural effusion related to the clinical profile of pulmonary hypertension and decompensated heart failure (Figure 3). In addition, technetium triphasic scintigraphy showed no increased radiotracer uptake in the lesion. The swab specimen revealed Gram-positive cocci in pairs, and culture was positive for multidrug-resistant Staphylococcus aureus and negative for fungi and mycobacteria after 70 days of incubation. The antibiotic regimen was changed to oxacillin. The result of the histopathological examination of the sternal lesion revealed caseous granuloma. For PCR analysis (Álvaro Laboratory, Cascavel, Brazil), a second sternal biopsy was performed, and the empirical treatment for TB using regimen I (rifampin, isoniazid and pyrazinamide) was initiated. The patient presented a favorable response. The PCR analysis was positive for Mycobacterium tuberculosis, confirming the diagnosis of tuberculous sternal osteomyelitis.
Discussion
Brazil ranks 14th among the 23 countries that, together, account for 80% of all TB cases worldwide, with a prevalence of 58 cases/100,000 population and an incidence of 47.2 cases/100,000 population.(3) Bone and joint involvement accounts for 1-3% of TB cases, and involvement of the sternum accounts for less than 1%.(4,5) Sternal TB predominantly affects young adult males, with or without predisposing factors, living in areas where TB is endemic.(2) Contamination can originate from infected local lymph nodes (contiguous with the lung parenchyma) or due to reactivation of a quiescent focus.(6)
The case described here reflects the indolent character of osteoarticular TB, in contrast to that of pyogenic osteomyelitis, caused principally by S. aureus, Pseudomonas aeruginosa, Salmonella sp. and Aspergillus sp., the latter being a disease that typically has an abrupt onset and prominent constitutional symptoms.(6) The clinical presentation, including symptoms such as sternal pain and swelling evolving over approximately one year, together with normal chest X-ray findings and an ESR of 48 mm/h, is in accordance with data reported in a case-series study of sternal TB, in which symptoms evolved over a mean of 9 months and the most common (in 81% of the cases) were sternal pain and swelling.(2) In that study, chest X-ray findings were normal in 73% of the cases and ESR was elevated (mean, 67 mm/h) in almost all cases.(2) Other reported cases have also shown a persistent increase in ESR.(4-7)
From a radiological standpoint, sternal TB can present the following patterns of bone destruction: osteolytic lesions; periosteal reaction; enhancement patterns; and soft tissue abscess with or without internal calcium formations.(6) These findings, which are not exclusive to sternal TB, can be found in aggressive infections such as actinomycosis.(8) Although CT does not appear to have any advantage over sternum X-ray in the evaluation of bone involvement, it is significantly superior in the evaluation of perilesional soft tissues, mediastinal involvement and pulmonary involvement.(5-9) Magnetic resonance imaging is a good option for the evaluation of soft tissues and bone lesions, revealing early alterations in the bone marrow, especially at early stages with normal X-ray findings.(4,5,9) Technetium triphasic scintigraphy has high sensitivity and specificity for the diagnosis of osteomyelitis.(2,4) In the case presented here, there was no increased radiotracer uptake in the sternum or photopenia in the osteolytic lesion, nor were there any other findings consistent with osteomyelitis.
In the present case, microbiological evaluation and cultures were negative, and the diagnosis was confirmed using PCR.(10) The histopathological finding of caseous granuloma was the principal evidence on which the working diagnosis was based. In one study, microbiological evaluation was positive for acid-fast bacilli in 38% of the cases, cultures were positive for M. tuberculosis in 85% of the cases, and typical granulomas were found in 67% of the cases.(1,2) According to the literature, the definitive diagnosis of sternal TB is based on microbiological evaluation together with histopathological confirmation.(6) Two groups of authors evaluating methods applied in the diagnosis of TB found that the sensitivity and specificity of PCR (90% and 80%, respectively) were similar to those of culture.(11,12) Both groups of authors stated that the quality of the sample and the standardization of the DNA extraction technique are critical factors in the applicability of PCR in the diagnosis of TB in Brazil. In the case reported here, it is likely that microbiological evaluation and culture were negative for acid-fast bacilli due to the bactericidal effect that ciprofloxacin has on M. tuberculosis.(13)
The principal differential diagnoses are malignancy, sarcoidosis, actinomycosis and fungal infections.(6,7) In the literature, there is no consensus regarding treatment modality, treatment duration or the best treatment regimen. Although early drainage and complete debridement improve cicatrization and prevent recurrence, some authors suggest that conservative treatment with antituberculous drugs be performed and surgical debridement be reserved for chronic cases with structural complications or for cases of treatment failure.(2,5,7) The use of prophylaxis in open heart surgery candidates with a history of TB or contact with TB is not indicated due to the rarity of the infection.(9) In our patient, treatment with regimen I resulted in clinical improvement and better cicatrization of the sternal lesion. At this writing, the patient was still under treatment. Surgical debridement was not considered due to the multiple comorbidities presented by the patient.
References
References
- 1. Ford SJ, Rathinam S, King JE, Vaughan R. Tuberculous osteomyelitis of the sternum: successful management with debridement and vacuum assisted closure. Eur J Cardiothorac Surg. 2005;28(4):645-7.
- 2. McLellan DG, Philips KB, Corbett CE, Bronze MS. Sternal osteomyelitis caused by mycobacterium tuberculosis: case report and review of the literature. Am J Med Sci. 2000;319(4):250-4.
- 3. Sociedade Brasileira de Pneumologia e Tisiologia. II Consenso Brasileiro de Tuberculose - Diretrizes Brasileiras para Tuberculose 2004. J Pneumol. 2004;30(Suppl 1): S1-S85.
- 4. Shah J, Patkar D, Parikh B, Parmar H, Varma R, Patankar T, et al. Tuberculosis of the sternum and clavicle: imaging findings in 15 patients. Skeletal Radiol. 2000;29(8):447-53.
- 5. Khan SA, Varshney MK, Hasan AS, Kumar A, Trikha V. Tuberculosis of the sternum: a clinical study. J Bone Joint Surg Br. 2007;89(6):817-20.
- 6. Atasoy C, Oztekin PS, Ozdemir N, Sak SD, Erden I, Akyar S. CT and MRI in tuberculous sternal osteomyelitis: a case report. Clin Imaging. 2002;26(2):112-5.
- 7. Bohl JM, Janner D. Mycobacterium tuberculosis sternal osteomyelitis presenting as anterior chest wall mass. Pediatr Infect Dis J. 1999;18(11):1028-9.
- 8. Khalil A, Le Breton C, Tassart M, Korzec J, Bigot J, Carette M. Utility of CT scan for the diagnosis of chest wall tuberculosis. Eur Radiol. 1999;9(8):1638-42.
- 9. Wang TK, Wong CF, Au WK, Cheng VC, Wong SS. Mycobacterium tuberculosis sternal wound infection after open heart surgery: a case report and review of the literature. Diagn Microbiol Infect Dis. 2007;58(2):245-9.
- 10. Clarridge JE 3rd, Shawar RM, Shinnick TM, Plikaytis BB. Large-scale use of polymerase chain reaction for detection of Mycobacterium tuberculosis in a routine mycobacteriology laboratory. J Clin Microbiol. 1993;31(8):2049-56.
- 11. Bollela VR, Sato DN, Fonseca BA. Problemas na padronização da reação em cadeia da polimerase para diagnóstico da tuberculose pulmonar. Rev Saude Publica. 1999;33(3):281-6.
- 12. Santos RM, Ogusku MM, Miranda JM, Dos-Santos MC, Salem JI. Evaluation of polymerase chain reaction in the diagnosis of pulmonary tuberculosis in indigenous and non-indigenous patients. J Bras Pneumol. 2006;32(3):234-40.
- 13. Gibbons FK, Branda JA, Shepard JA. Case records of the Massachusetts General Hospital. Case 12-2006. A 37-year-old man with hemoptysis and a pulmonary infiltrate. N Engl J Med. 2006;354(16):1729-37.

 Sternal osteomyelitis caused by infection with Mycobacterium tuberculosis
Sternal osteomyelitis caused by infection with Mycobacterium tuberculosis