Abstract
Here we describe an infrequent case of gastrointestinal stromal tumor of the rectum in a 57 year-old man with spindle cell neoplasm probably gastrointestinal stromal tumor and CT scan showed tumor from the anterior rectal wall and offered abdominoperineal resection for the same. The patient was started on imatinib and had a significant reduction in symptoms. The patient was reassessed with the CT scan, which showed a reduction in tumor size and Transanal minimally invasive surgery was planned for the patient. Use of imatinib prior to surgical resection to attain the reduced size of the tumor within the limit of resection is an attractive approach. Since tumor development can happen rapidly again after substantial tumor shrinkage, the best time to operate depending on resectability and the maximum therapeutic outcome remains divisive.
Keywords: Rectal gastrointestinal stromal tumor; Neoadjuvant imatinib; TAMIS
Resumo
No presente estudo, os autores descrevem um caso raro de tumor estromal gastrointestinal no reto em um homem de 57 anos que se apresentou com neoplasia de células fusiformes, com provável tumor estromal gastrointestinal. A tomografia computadorizada demonstrou tumor na parede anterior do reto e foi sugerida sua ressecção abdominoperineal. O paciente iniciou tratamento com imatinibe e apresentou uma redução significativa nos sintomas. O paciente foi reavaliado por tomografia computadorizada, que evidenciou redução do tamanho do tumor; portanto, foi indicada cirurgia transanal minimamente invasiva. O tumor era ressecável e foi necessário um extenso acompanhamento para romper o órgão, de forma a alcançar a ressecção máxima; caso contrário, o tumor estromal gastrointestinal também seria irressecável. O uso de imatinibe antes da ressecção cirúrgica para reduzir o tamanho do tumor dentro do limite de ressecção é uma abordagem interessante. Como o tumor pode se crescer rapidamente após ser substancialmente reduzido, a literatura ainda apresenta controvérsias quanto ao melhor momento para operar e quanto ao melhor desfecho terapêutico.
Palavras-chave: Tumor estromal gastrointestinal no reto; Imatinibe neoadjuvante; TAMIS
Introduction
A gastrointestinal stromal tumor (GIST) is an infrequent tumor of the gastrointestinal tract which is rare in case of rectum origin. The commonest site of GIST is stomach, small bowel, a colon followed by esophagus.1,2 Rectal GIST constitutes 0.1% of GI tumors. The occurrence of mesenchymal tumor in the GI tract is less common with an incidence of 6.8 million annually according to a current epidemiological study from the USA.3,4 GIST arising from interstitial cells of Cajal expresses CD117 (c-kit proto-oncogene), CD34 and DOG1, which are detected immunohistochemically for diagnostic confirmation.5
The mainstay of treatment in rectal GIST is surgery with clear resection of margins as gold standard treatment.6 Neoadjuvant/adjuvant and/or Imatinib therapy are prescribed according to different situations.7 Imatinib plays a role in adjuvant setting as well as a metastatic disease; however, its function in the neoadjuvant setting is not established well. However in rectal GIST especially when it is bulky neoadjuvant therapy with imatinib will be useful in downsizing and downstaging the disease for sphincter preservation. Imatinib, a tyrosine kinase inhibitor initially used in chronic myeloid leukemia treatment delivered with good results has revolutionized the management of GIST treatment also.8–12 In this report, we describe an infrequent case of GIST of the rectum in a 57-year-old man who underwent transanal minimally invasive surgery after tumor size was reduced with neoadjuvant imatinib 400 mg OD for 3 months.
Case report
A 57-year-old male presented with complaints of bleeding per rectum, constipation, and mass descending per rectum for 6 months with no other constitutional symptoms or comorbid illness. On examination, the patient was found to be pale and no mass was palpable on abdominal examination. Rectal examination revealed a polypoidal mass in the anterior wall which was 3–4 cm from the anal verge, which was mobile, firm in consistency, bled on touch an upper limit could not be reached.
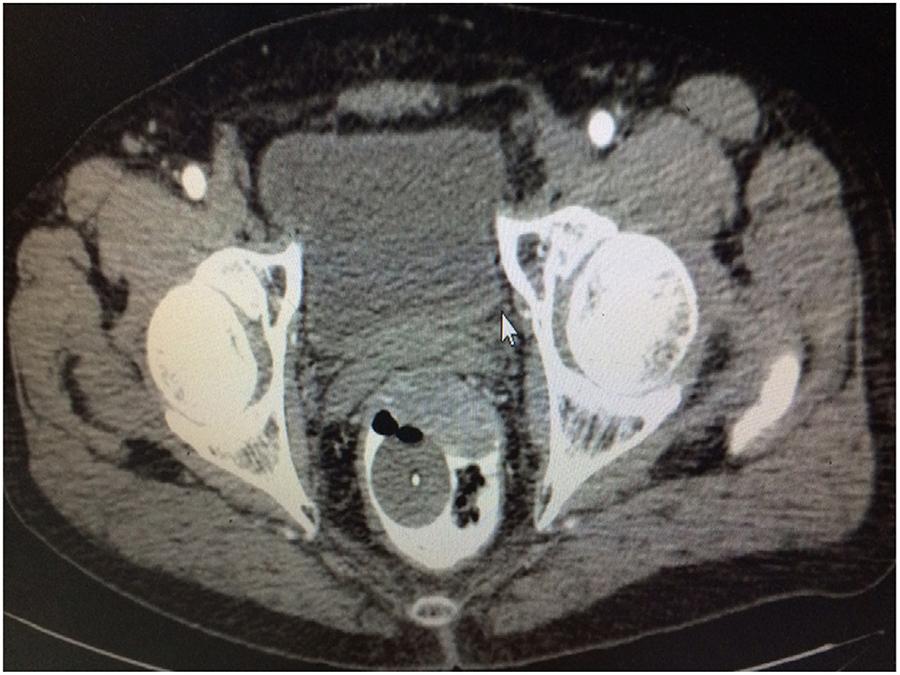
At first, the patient was evaluated in OPD clinic, on investigating his hemoglobin was found to be 7.9 gms/dL, coagulation profile, renal and liver function tests were within normal limits. An earlier checkup in another hospital for the same with Colonoscopy with biopsy which showed spindle cell neoplasm probably GIST (Immunohistochemistry not done) and CT scan showed tumor from anterior rectal wall measuring 8.3 × 7 × 7.7 cm (Figs. 1 and 2). The patient was offered abdominoperineal resection for the same.
Preoperative CT scan showing rectal GIST occupying the entire rectum (before neoadjuvant imatinib).
Patient came for the second opinion and was desperate for sphincter preservation. Repeat colonoscopy and biopsy was done in our institution which showed GIST of low malignant potential, IHC being positive for CD117 (Fig. 3), DOG1, Vimentin. Initially, it was planned for downsizing tumor; the patient was started on imatinib 400 mg 0D for 3 months. The patient was on regular follow-up every month, he had a significant reduction in symptoms after starting the therapy, and he became asymptomatic after 3 months of therapy.
The patient was reassessed with the CT scan, which showed a reduction in tumor size to 3.8 × 2.1 × 3.7 cm (Fig. 4). Fig. 5a and 5b shows the coronal and sagittal section of CT showing tumor after neoadjuvant therapy. Since the size decreased, we planned for TAMIS (Transanal Minimally Invasive Surgery) for the patient. The patient was placed in a prone position due to the anterior placement of the tumor; Single-incision laparoscopic port was used for the surgery. The harmonic scalpel was used for the dissection; a full thickness excision of the anterior wall involving GIST with adequate negative margin was performed. The raw area of the rectum was closed with V-Lock stitch. The postop period was uneventful. Enteral feeding was started on the first post-op day and the patient was discharged on the fourth post-op day. Final biopsy report showed ypT2pNxcM0 with Grade 1 GIST spindle type, with margins being free of tumor and the mitotic rate was 4/50 HPF. The patient was started on postop Imatinib therapy; he is on regular follow-up every 3 months.
Preoperative CT scan after imatinib therapy showing a reduction in the size of rectal GIST compared to previous CT scan.
Discussion
GIST is an infrequent mesenchymal tumor and incidence of rectal GIST is a rare occurrence. GIST is considered to be originating from interstitial cells of Cajal-like which have been reported from several extraintestinal organs. The symptoms of GIST in the rectum shows similar characteristic to rectal tumors and a diagnostic investigation is analogous to other rectal mass. The frequency of rectal GIST is scanty compared to GIST of other GI organs like stomach or intestine and hence the clinical-pathological details of rectal GIST are not verified or established completely.2,5 With the available literature, it is now considered that rectal GIST patients usually have bleeding per rectum, constipation, tenesmus together with pelvic pain. Apart from this, they might also have mass palpable per rectum during examination.13,14
Various radiological examinations are performed to establish the diagnosis of GIST includes colonoscopy, MRI to assess the tumor and sphincter complex and CT scan to look for metastasis. Role of MRI or PET scan in GIST is mainly to assess the metastasis and response to treatment. Colonoscopy also provides with sample for biopsy to know the type of tumor and mitotic activity. Rectal GIST has a very similar clinical profile like other GIST, therefore there is a predisposition to authenticate the same prognostic factors for rectal GIST as for other GIST of different sites, particularly gastric GIST. Diagnosis includes digital assessment of the rectum, colonoscopy, and transrectal ultrasound together with preoperative biopsy. A definite diagnosis is difficult without the presence of mucosal invasion or extrinsic deformity, and thus endoscopy provides the diagnostic biopsy material alone.9,10,13,14
GIST characteristically expresses CD117; often CD34 and their expressions vary depending on the origin of sites. GIST located all through the gastrointestinal tract, express CD117, a most important GIST marker which also a target for drug therapy with imatinib, which is a tyrosine-kinase receptor inhibitor. Although imatinib is a promising chemotherapeutic drug for highly developed GIST, total surgical resection remains the most successful treatment for such a tumor.15 Due to restricted space in the pelvis area, the treatment of GIST of rectal origin has limited option for treatment and patient may require abdominoperineal resection. So before any surgical procedure, it is considered to downsize tumor, preserve the anal sphincter using imatinib.16–18 In randomized, trials 70% response rate for imatinib was noted in unresectable and metastatic GIST. Another study among 161 patients having locally advanced GISTs showed a good response to neoadjuvant imatinib treatment with 80% response rate.19
TAMIS (Transanal Minimally Invasive Surgery) is a minimally invasive technique used in the treatment of rectal lesions that avoids conventional pelvic surgery or laparotomy. Advantage of TAMIS over TEMS (Transanal Endoscopic Microsurgery) is the availability of laparoscopic instruments universally, no need for special dedicated instruments. In general, in the post-operative management of tumors at high risk and/or in cases of incomplete surgical resection, therapy with imatinib or adjuvant imatinib is also suggested. Although more or less it is now accepted that imatinib is a suitable treatment for metastatic tumors even at an advanced stage, further in-depth analysis of treatment efficiency with this drug is required in patients with high-risk tumors with the neoadjuvant therapy.7,13,20,21
Use of imatinib prior to surgical resection to attain the reduced size of the tumor within the limit of resection is an attractive approach. In general, therapeutic schedule for a course of imatinib is 3–12 months, which require frequent imaging studies and a re-evaluation to decide the most appropriate time for surgery. Since tumor development can happen rapidly again after substantial tumor shrinkage, the best time to operate depending on resectability and the maximum therapeutic outcome remains divisive.
In conclusion, rectal GIST although it is extremely rare, it can be treated by means of differential diagnosis. Rectal GIST follows the very similar diagnostic work-up as advised for any other rectal neoplasia. Since the immunohistochemical characterization of CD117 and CD34 is almost required to reach a certain preoperative diagnosis hence biopsy of the tumor is a necessary diagnostic procedure. A series of patients followed for a long time under observations would make it easy to assess the post-surgical resection for rectal GIST which would further help to ascertain the most efficient treatment strategy for rectal GIST.
References
- 1 Corless CL, Fletcher JA, Heinrich MC. Biology of gastrointestinal stromal tumors. J Clin Oncol. 2004;22:3813-25.
- 2 Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: An analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 2005;100:162-8.
- 3 Gatta G, Van Der Zwan JM, Casali PG, Siesling S, Dei Tos AP, Kunkler I, et al. Rare cancers are not so rare: the rare cancer burden in Europe. Eur J Cancer. 2011;47:2493-511.
- 4 Demetri GD, Von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010;8(Suppl 2):S-1.
- 5 Steigen SE, Eide TJ. Gastrointestinal stromal tumors (GISTs): a review. Apmis. 2009;117:73-86.
- 6 Jakob J, Mussi C, Ronellenfitsch U, Wardelmann E, Negri T, Gronchi A, et al. Gastrointestinal stromal tumor of the rectum: results of surgical and multimodality therapy in the era of imatinib. Ann Surg Oncol. 2013;20:586-92.
- 7 France Neto PR, Ramos LA, Silva LC, Fernandes CK, Lacerda-Filho A. Neoadjuvant use of imatinib mesylate for treatment of large rectal GIST: case report. Braz J Coloproctol. 2011;31:89-93.
- 8 Heinrich MC, Corless CL, Demetri GD, Blanke CD, Von Mehren M, Joensuu H, et al. Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol. 2003;21:4342-9.
- 9 Machlenkin S, Pinsk I, Tulchinsky H, Ziv Y, Sayfan J, Duek D, et al. The effect of neoadjuvantimatinib therapy on outcome and survival after rectal gastrointestinal stromal tumour. Colorectal Dis. 2011;13:1110-5.
- 10 Nozawa H, Kanazawa T, Tanaka T, Takahashi M, Ishihara S, Sunami E, et al. Laparoscopic resection of a gastrointestinal stromal tumor of the lower rectum in a patient with coronary artery disease following long-term neoadjuvantimatinib treatment and anticoagulation therapy. World J Surg Oncol. 2014;12:211.
- 11 Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, et al. Laparoscopic local excision and rectoanal anastomosis for rectal gastrointestinal stromal tumor: modified laparoscopic intersphincteric resection technique. Dis Colon Rectum. 2014;57:900-4.
- 12 Rutkowski P, Gronchi A, Hohenberger P, Bonvalot S, Schöffski P, Bauer S, et al. Neoadjuvantimatinib in locally advanced Gastrointestinal Stromal Tumors (GIST): the EORTC STBSG experience. Ann Surg Oncol. 2013;20:2937-43.
- 13 Eisenberg BL, Trent JC. Adjuvant and neoadjuvant imatinib therapy: current role in the management of gastrointestinal stromal tumors. Int J Cancer. 2011;129:2533-42.
- 14 Arezzo A, Verra M, Morino M. Transanal endoscopic microsurgery after neoadjuvant therapy for rectal GIST. Dig Liver Dis. 2011;43:921-4.
- 15 Salazar M, Barata A, André S, Venâncio J, Francisco I, Cravo M, et al. First report of a complete pathological response of a pelvic GIST treated with imatinib as neoadjuvant therapy. Gut. 2006;55:585-6.
- 16 Machlenkin S, Pinsk I, Tulchinsky H, Ziv Y, Sayfan J, Duek D, et al. The effect of neoadjuvant imatinib therapy on outcome and survival after rectal gastrointestinal stromal tumour. Colorectal Dis. 2011;13:1110-5.
- 17 Fiore M, Palassini E, Fumagalli E, Pilotti S, Tamborini E, Stacchiotti S, et al. Preoperative imatinibmesylate for unresectable or locally advanced primary gastrointestinal stromal tumors (GIST). Eur J Surg Oncol. 2009;35:739-45.
- 18 Hamada M, Ozaki K, Horimi T, Tsuji A, Nasu Y, Iwata J, et al. Recurrent rectal GIST resected successfully after preoperative chemotherapy with imatinibmesylate. Int J Clin Oncol. 2008;13:355-60.
- 19 Lo SS, Papachristou GI, Finkelstein SD, Conroy WP, Schraut WH, Ramanathan RK. Neoadjuvantimatinib in gastrointestinal stromal tumor of the rectum: report of a case. Dis Colon Rectum. 2005;48:1316-9.
- 20 Rutkowski P, Gronchi A, Hohenberger P, Bonvalot S, Schöffski P, Bauer S, et al. Neoadjuvantimatinib in locally advanced gastrointestinal stromal tumors (GIST): the EORTC STBSG experience. Ann Surg Oncol. 2013;20:2937-43.
- 21 Nahas SC, Nahas CS, Marques CF, Dias AR, Pollara WM, Cecconello I. Transanal Endoscopic Microsurgery (TEM): a minimally invasive procedure for treatment of selected rectal neoplasms. Arq Bras Cir Dig. 2010;23:35-9.
Publication Dates
-
Publication in this collection
23 Mar 2020 -
Date of issue
Jan-Mar 2020
History
-
Received
14 May 2019 -
Accepted
29 July 2019 -
Published
13 Sept 2019
 A rectal gastrointestinal stromal tumor—a plea for neoadjuvant imatinib and TAMIS
A rectal gastrointestinal stromal tumor—a plea for neoadjuvant imatinib and TAMIS