Abstracts
The analysis of 2,840 cases of hemorrhoidectomy by open techniques of Milligan-Morgan (2,189 cases), Ferguson (341 cases) and mixed (310 cases) in 11,043 patients with hemorrhoidal disease (HD) allowed the following conclusions. The patients' acceptance of surgical indication for hemorrhoidectomy was 25.7%. Hemorrhoidectomy was more common among women (53.8%) than men (46.2%), and more accepted by women (26.5%) than men (24.8%). Hemorrhoidectomy was more common in patients of the fourth (27.7%), fifth (21.9%) and third (21.0%) decades of age. Most patients who agreed to undergo hemorrhoidectomy were those of the second (38.2%), eighth (35.9%) and ninth (34.5%) decades of age. The overall incidence of surgical complications was 3.0% (87 cases): anal stenosis (1.8%), bleeding (0.8%), worsening of anal hypotonia (0.2%), sepsis (0.1%) and systemic complications (0.1%), with no difference among the techniques used. The incidence of surgical complications by Milligan-Morgan technique was 3.0% - stenosis (1.9%), bleeding (1.9%), worsening of anal hypotonia (0.2%) and systemic complications (0.04%). The incidence of surgical complications by Ferguson's technique was 3.5% - stenosis (1.7%), bleeding (0.6%), worsening of anal hypotonia (0.6%) and sepsis (0.6%). And the incidence of surgical complications by mixed techniques was 2.5% - stenosis (1.0%), bleeding (0.3%), worsening of anal hypotonia (0.3%), sepsis (0.3%) and systemic complications (0.3%). The incidence of surgical complications according to gender was 3.0% among women and 3.2% among men, with higher incidence of stenosis in women (2.0%) and hemorrhage in men (1.1%). Surgical complications were more observed in the eighth (5.1%) and seventh (3.8%) decades of age. The incidence of anal stenosis was 1.8%, being 64.0% without hypotonia and 66.0% without anal fissure (66.0%), with annular stenosis as the most common anatomical shape (70.0%). Anal stenosis was more common among women (2.0%) presenting mean age of 38.2 years, with no relation to age decades. The most common technique for anal stenosis was single anotomy without sphincterotomy (46.0%). All cases of anal bleeding had surgical ligation of all hemorrhoidal pedicles, no matter if the bleeding site was found or not.
gastrointestinal hemorrhage; hemorrhoids; hemorrhoids/epidemiology statistical analysis
O seguimento de uma casuística de 2.840 hemorroidectomias pelas técnicas de Milligan-Morgan (2.189 casos), Ferguson (341 casos) e mista (310 casos) em 11.043 pacientes portadores de doença hemorroidária (DH) permitiu as seguintes conclusões. A aceitação da indicação cirúrgica para doença hemorroidária (DH), pelos pacientes, foi de 25,7%. A doença hemorroidária (DH) foi mais comum entre mulheres (53,8%) que em homens (46,2%) e a hemorroidectomia foi mais aceita pelas mulheres (26,5%) que pelos homens (24,8%). A hemorroidectomia foi mais realizada em pacientes de quarta (27,7%), quinta (21,9%) e terceira (21,0%) décadas etárias. Os pacientes que mais aceitaram a indicação cirúrgica foram os da segunda (38,2%), oitava (35,9%) e nona (34,5%) décadas etárias. A incidência global de complicações cirúrgicas foi de 3,0% (87 casos): estenose anal (1,8%), hemorragia grave (0,8%), agravamento da hipotonia anal (0,2%), sepse (0,1%) e sistêmicas (0,1%), sem diferença entre as técnicas usadas. A incidência de complicações cirúrgicas pela técnica de Milligan-Morgan foi de 3,0%: estenose (1,9%), hemorragia grave (1,9%), agravamento da hipotonia anal (0,2%) e sistêmicas (0,04%). A incidência de complicações cirúrgicas pela técnica de Ferguson foi de 3,5%: estenose (1,7%), hemorragia grave (0,6%), agravamento da hipotonia anal (0,6%) e sepse (0,6%). A incidência de complicações cirúrgicas pela técnica mista foi de 2,5%: estenose (1,0%), hemorragia grave (0,3%), agravamento da hipotonia anal (0,3%), sepse (0,3%) e sistêmicas (0,3%). A incidência de complicações cirúrgicas pelos gêneros foi de 3,0% entre as mulheres e 3,2% entre os homens, com maior incidência de estenose nas mulheres (2,0%) e hemorragia nos homens (1,1%). As décadas em que mais ocorreram complicações foram a oitava (5,1%) e a sétima (3,8%). A incidência de estenose anal foi de 1,8%, prevalecendo sem hipertonia anal (64,0%) e com fissura anal (66,0%), sendo a forma anatômica mais comum a anular (70,0%); foi mais comum entre mulheres (2,0%) com idade média de 38,2 anos, sem relação com as décadas etárias. A cirurgia corretiva da estenose anal mais usada foi a anotomia simples ou com fissurectomia sem esfincterotomia (46,0%). Em todos os casos de hemorragia anal cirúrgica foi feita ligadura de todos os pedículos da ressecção hemorroidária, independentemente de se encontrar ou não o local da hemorragia.
hemorragia gastrintestinal; hemorroidas; hemorroidas/epidemiologia; análise estatística
ORIGINAL ARTICLE
Surgical complications in 2,840 cases of hemorrhoidectomy by Milligan-Morgan, Ferguson and combined techniques
Guilherme de Almeida SantosI; Caroline Pinto CoutinhoI; Matheus Matta Machado Mafra Duque Estrada MeyerI; Diego Vieira SampaioI; Geraldo Magela Gomes da CruzII
IResident Physicians Specializing in the Group of Coloproctology at Santa Casa de Belo Horizonte (SCBH) Belo Horizonte (MG), Brazil
IIDoctor in Surgery; Full Professor of Coloproctology at the Faculdade de Ciências Médicas de Minas Gerais (FCMMG); Full Professor of the Postgraduate and Research Program of the Instituto de Ensino e Pesquisa at SCBH; Coordinator of the Group of Coloproctology at SCBH; Honorary Member at the Sociedade Brasileira de Coloproctologia (SBCP)
Correspondence to Correspondence to: Geraldo Magela Gomes da Cruz Rua Rio de Janeiro, 2.017, apto. 1.401 Lourdes 30160-042 Belo Horizonte (MG), Brazil E-mail: magelacruz@terra.com.br
ABSTRACT
The analysis of 2,840 cases of hemorrhoidectomy by open techniques of Milligan-Morgan (2,189 cases), Ferguson (341 cases) and mixed (310 cases) in 11,043 patients with hemorrhoidal disease (HD) allowed the following conclusions. The patients' acceptance of surgical indication for hemorrhoidectomy was 25.7%. Hemorrhoidectomy was more common among women (53.8%) than men (46.2%), and more accepted by women (26.5%) than men (24.8%). Hemorrhoidectomy was more common in patients of the fourth (27.7%), fifth (21.9%) and third (21.0%) decades of age. Most patients who agreed to undergo hemorrhoidectomy were those of the second (38.2%), eighth (35.9%) and ninth (34.5%) decades of age. The overall incidence of surgical complications was 3.0% (87 cases): anal stenosis (1.8%), bleeding (0.8%), worsening of anal hypotonia (0.2%), sepsis (0.1%) and systemic complications (0.1%), with no difference among the techniques used. The incidence of surgical complications by Milligan-Morgan technique was 3.0% stenosis (1.9%), bleeding (1.9%), worsening of anal hypotonia (0.2%) and systemic complications (0.04%). The incidence of surgical complications by Ferguson's technique was 3.5% stenosis (1.7%), bleeding (0.6%), worsening of anal hypotonia (0.6%) and sepsis (0.6%). And the incidence of surgical complications by mixed techniques was 2.5% stenosis (1.0%), bleeding (0.3%), worsening of anal hypotonia (0.3%), sepsis (0.3%) and systemic complications (0.3%). The incidence of surgical complications according to gender was 3.0% among women and 3.2% among men, with higher incidence of stenosis in women (2.0%) and hemorrhage in men (1.1%). Surgical complications were more observed in the eighth (5.1%) and seventh (3.8%) decades of age. The incidence of anal stenosis was 1.8%, being 64.0% without hypotonia and 66.0% without anal fissure (66.0%), with annular stenosis as the most common anatomical shape (70.0%). Anal stenosis was more common among women (2.0%) presenting mean age of 38.2 years, with no relation to age decades. The most common technique for anal stenosis was single anotomy without sphincterotomy (46.0%). All cases of anal bleeding had surgical ligation of all hemorrhoidal pedicles, no matter if the bleeding site was found or not.
Keywords: gastrointestinal hemorrhage; hemorrhoids; hemorrhoids/epidemiology statistical analysis.
RESUMO
O seguimento de uma casuística de 2.840 hemorroidectomias pelas técnicas de Milligan-Morgan (2.189 casos), Ferguson (341 casos) e mista (310 casos) em 11.043 pacientes portadores de doença hemorroidária (DH) permitiu as seguintes conclusões. A aceitação da indicação cirúrgica para doença hemorroidária (DH), pelos pacientes, foi de 25,7%. A doença hemorroidária (DH) foi mais comum entre mulheres (53,8%) que em homens (46,2%) e a hemorroidectomia foi mais aceita pelas mulheres (26,5%) que pelos homens (24,8%). A hemorroidectomia foi mais realizada em pacientes de quarta (27,7%), quinta (21,9%) e terceira (21,0%) décadas etárias. Os pacientes que mais aceitaram a indicação cirúrgica foram os da segunda (38,2%), oitava (35,9%) e nona (34,5%) décadas etárias. A incidência global de complicações cirúrgicas foi de 3,0% (87 casos): estenose anal (1,8%), hemorragia grave (0,8%), agravamento da hipotonia anal (0,2%), sepse (0,1%) e sistêmicas (0,1%), sem diferença entre as técnicas usadas. A incidência de complicações cirúrgicas pela técnica de Milligan-Morgan foi de 3,0%: estenose (1,9%), hemorragia grave (1,9%), agravamento da hipotonia anal (0,2%) e sistêmicas (0,04%). A incidência de complicações cirúrgicas pela técnica de Ferguson foi de 3,5%: estenose (1,7%), hemorragia grave (0,6%), agravamento da hipotonia anal (0,6%) e sepse (0,6%). A incidência de complicações cirúrgicas pela técnica mista foi de 2,5%: estenose (1,0%), hemorragia grave (0,3%), agravamento da hipotonia anal (0,3%), sepse (0,3%) e sistêmicas (0,3%). A incidência de complicações cirúrgicas pelos gêneros foi de 3,0% entre as mulheres e 3,2% entre os homens, com maior incidência de estenose nas mulheres (2,0%) e hemorragia nos homens (1,1%). As décadas em que mais ocorreram complicações foram a oitava (5,1%) e a sétima (3,8%). A incidência de estenose anal foi de 1,8%, prevalecendo sem hipertonia anal (64,0%) e com fissura anal (66,0%), sendo a forma anatômica mais comum a anular (70,0%); foi mais comum entre mulheres (2,0%) com idade média de 38,2 anos, sem relação com as décadas etárias. A cirurgia corretiva da estenose anal mais usada foi a anotomia simples ou com fissurectomia sem esfincterotomia (46,0%). Em todos os casos de hemorragia anal cirúrgica foi feita ligadura de todos os pedículos da ressecção hemorroidária, independentemente de se encontrar ou não o local da hemorragia.
Palavras-chave: hemorragia gastrintestinal; hemorroidas; hemorroidas/epidemiologia; análise estatística.
INTRODUCTION TO SURGICAL TREATMENT OF HEMORRHOIDAL DISEASE
For Thomson1, hemorrhoidal disease (HD) is "an anatomical and pathophysiologic alteration, characterized by loss of elasticity and increased volume of the structures of hemorrhoidal cushions, which causes cushion swelling, vascular dilation and displacement". Then, the treatment of HD includes reduction of volume of these tissues and fixation of adjacent tissues.
Besides the clinical approaches (general and local care, hygienic and dietetic measures and medication), there are techniques called "non-surgical interventions" and "surgical interventions" (Table 1) to treat this disease.
Non-surgical interventions
The techniques called "non-surgical interventions" address HD above the pectineal line, an endodermic region without cerebrospinal or reflexive innervation, and do not cause pain. They include sclerotherapy2, rubber band ligation (RBL)3,4, macro rubber band ligation4, photocoagulation4, cryotherapy2 and Doppler-guided hemorrhoidal artery ligation4. Sclerotherapy2 destroys internal hemorrhoids using chemical agents; photocoagulation4 through the application of electricity that crosses the liquid crystal; cryotherapy2 through freezing, with the application of nitrogen; RBL3,4 through mechanical strangling using a rubber band; and Doppler-guided hemorrhoidal artery ligation4 uses artery occlusion to destroy internal hemorrhoids. All these techniques are used in the region above the pectineal line. Besides, these techniques, after the process of fibrosis following necrosis, secondarily lead to fixation of adjacent tissues to the hemorrhoids. RBL3,4 strangles internal hemorrhoids, which, due to absent irrigation, end up "removed" by tissue necrosis; not acting on the external component.
Surgical interventions
The "surgical interventions" are divided into two groups: techniques that include fixation of the hemorrhoidal cushions without removing the hemorrhoids (clamping, such as the procedure for prolapsed hemorrhoids PPH)4-7 and techniques that include the removal of tissues and hemorrhoidal arteries (hemorrhoidectomy). The second group includes several techniques, according to the method of tissue removal: open techniques (Milligan-Morgan8 and its variations)2,4,9-13, closed techniques (Ferguson14 and its variations)2,4,15-18, amputative techniques (Whitehead19,20 and its variations)4,21, semi-closed techniques (Sokol4,22, Ruiz-Moreno4,23, René-Obando24 and René-Obando-Reis Neto4), submucosal techniques (Parks25)4,26 and association of RBL with resection of external hemorrhoids (Santos4,27) (Table 2).
Regardless of the technique used, hemorrhoidectomy can be classified according to the cutting, dissection and hemostasis instruments used by the expert: cold blade, electrocauterization2,4, cryo2, CO2/YAG laser4,13,28,29, harmonic scalpel4,7,30.
The PPH6,4,12,31 removes an annular and circular portion of the mucosa and submucosa from the region above the pectineal line, lifting and fixing the hemorrhoidal vessels that would also interrupt blood flow in case of persistent external hemorrhoids.
Hemorrhoidectomy means the removal of internal and external hemorrhoids, with subsequent fixation of adjacent tissues, eliminating the symptoms presented by the patient with HD and the physical findings diagnosed before the surgery. Then, the difference between "hemorrhoidectomy" and "non-surgical invasive treatment of HD" lies in the fact that, in the first, internal and external hemorrhoids are resected, removed, extirpated, with subsequent fixation of adjacent tissues, and in the second, the hemorrhoids are not resected.
Hemorrhoidectomy is the surgery for HD eradication that involves resection of cutaneous external hemorrhoids and mucosal internal hemorrhoids by cutting the skin around them, ligation and excision of internal and external hemorrhoids, which, in theory, may be used in any HD, regardless of its form and degree of progress. It may be performed by leaving the cutaneous and mucosal edges without suture, with the raw area closed by secondary intention (open hemorrhoidectomy); by suturing the cutaneous and mucosal edges (closed hemorrhoidectomy) or by suturing a portion of the raw areas (semi-closed hemorrhoidectomy). Table 2 shows the various non-surgical and surgical techniques for HD treatment.
Open hemorrhoidectomy (Milligan-Morgan8)
It has become a classic in the coloproctologic literature8 and a classical technique, largely used around the globe, undoubtedly, the most frequently used by experts worldwide (Figure 1). It basically involves the hemorrhoidal tissue excision, from the skin towards the mucosa, with ligation of vascular pedicle and the raw area of dissection to be closed by secondary intention, repeating this action as many times as necessary to resect all hemorrhoids. Hundreds of personal alterations have been introduced by the experts, with residents changing the recently-learned technique as the common practice. The changes vary from the patient's position on the operating table to the type of anesthesia, intestinal preparation or not, type of suture for pedicle and vessel ligation, cutting instrument (scalpel, scissors, cautery, laser, etc.), the direction of resection (from the skin towards the mucosa or the opposite).
The Milligan-Morgan technique31 is widely used worldwide2,4,9-13. We will discuss results and complications of this technique published in some studies.
Closed hemorrhoidectomy (Ferguson14)
This is another classical technique in the coloproctologic literature14. And, just like the open technique, it has become a largely used technique around the globe (Figure 2). It basically involves the hemorrhoidal tissue excision, from the skin towards the mucosa, with vascular pedicle ligation, similar to the Milligan-Morgan technique, but the areas of hemorrhoid resections are sutured, and not left open, with the cutaneous and mucosal edges placed together through running suture.
Just like the Milligan-Morgan technique8, this closed technique of Ferguson13 is widely used by the experts2,4,15-18. We will discuss results and complications of this technique published in some studies.
Mixed hemorrhoidectomy technique (closed and open areas)
Used by experts in both closed and open techniques, in case of excess or absence of skin in the raw areas of hemorrhoidectomy. Then, if using the open technique, the expert may close the resection to heal the wound and prevent anal skin tags due to excess skin; on the other hand, the expert that uses the closed technique may leave an open area due to absent skin that will act as a draining area.
Semi-closed technique (Sokol)
In the 1970's, Sokol22 developed a variation from the closed technique of Ferguson, popularly known in the medical community as Borba et al.4,22. It basically involves suture at the base of the hemorrhoid, which is repaired for subsequent use, a V-shaped mucocutaneous flap is made, with the hemorrhoid dissected until near the previously suture; the residual skin is sutured onto the wound at the V base with the previous suture; and the skin edges and mucosa are joined with running suture. In a series of 322 cases, Borba et al.4,22 did not observe relevant postoperative complications, but only two cases of anal sub-stenosis (0.6%).
Semi-closed technique (Ruiz-Moreno23)
After the resection of hemorrhoids, the mucosa and skin in the raw area are fixed through running suture, leaving it close to the midline, reducing the raw surface and allowing clean wound, with closed edges, which promotes healing. The purpose is to reduce the raw area, shortening the healing time and preventing anal skin tag in the postoperative period. It is similar to submucosal hemorrhoidectomy of Parks24, except for a basic aspect: marsupialization of the external part of the wounds; then, this is a semi-closed technique. The results of this surgery are similar to those described for closed hemorrhoidectomy4.
Semi-closed technique of René Obando24 and René Obando-Reis Neto4
The surgery involves the pectineal line repair, in which the internal hemorrhoid is forced outwards, becoming fully exposed; and then the repair of rectal mucosa, in the upper limit of the internal hemorrhoid; three or four full-thickness sutures are made radially, involving the mucosa and submucosa, along the craniocaudal length of the hemorrhoid to be resected; the mucosa and submucosa are cut between the ligations; the external part of the skin plexus is removed until the pectineal line with a V-shaped incision or a racket incision with external base. This technique is perfect for the approach to voluminous and proximally extended internal hemorrhoids, whose full dissection would cause a very high resection of the rectal mucosa, which involves inconvenient aspects.
Submucosal technique of Parks25
This technique, described by Alan Parks25, includes hemorrhoidectomy with preservation of the anal canal mucosa, reducing the surgical wound dimensions and leading to a shorter healing time, as well as lower stenosis indexes than those with conventional techniques. The surgery starts with the application of Parks retractor and injection of adrenaline solution at the dilution of 1:250.000 to reduce bleeding; after that, a Y-shaped incision is made at the mucocutaneous junction, between the upper mucosa of the anal canal and the anorectal junction, as an inverted racket incision; the vascular pedicle is separated from the mucosa and the sphincter plane, connecting it afterwards; the mucosa is closed with running suture, leaving a small area open in the perianal region for draining. The largest series with this technique was reported by Milito26, with 1,315 patients, admitting 82 cases of recurrences (7%), 75 cases of anal skin tag (6.5%), 19 cases of anal stenosis (1.6%), 36 cases of gas incontinence (3.2%). The fact that the mucosa is not included in the ligation leads to reduced postoperative pain. However, the surgical time is longer, the recurrence rate is higher and it involves greater risk of bleeding during the surgery and postoperatively.
Amputative technique of Whitehead19,20
Whitehead19,20 presented a series of 300 patients that, in 1887, were submitted to the technique that he developed, with good results. The surgery starts with the perianal skin elevation with Allis clamps to expose the terminal portion of the anal canal. Dissection is started right above the pectineal line, along the circumference, delimitating the skin portion to be used later as a flap; deep dissection is performed, until the external sphincter and the lower edge of the internal sphincter are seen; Allis clamps are removed, which are replaced at the distal edge of the dissection to allow the excess skin to be elevated; care should be taken to prevent artery removal from the cutaneous flap to be used later; the hemorrhoid dissection is performed until their upper edge; with Allis clamps, the dissected mucosal prolapse is pulled and divided into four quadrants, with a longitudinal incision, until the point where the mucosa dissection ended; excess perianal skin is gently taken into the anal canal, without stress, making the mucocutaneous suture, in such way to cover the anal canal; fixation is performed with polyglycolic acid, which should be anchored to the internal sphincter muscle of the anus, and then successively at the four points of deeper dissection, and each of these four points should be at slightly different levels, avoiding the running line, which may cause anal stenosis; the transected mucosal prolapse is sectioned between each of the four points previously established. Then, the mucocutaneous suture is made, with interrupted suture of polyglycolic acid, repeating the mucocutaneous suture of the other quadrants; in case of excess perianal skin, it should be radially resected, creating a drainage area.
Although many experts criticize the Whitehead technique, others attribute negative results to inadequate use of the technique, and not to the technique per se. Wollf and Culp21 and Cruz et al.4 defend the use of the Whitehead technique, provided that the procedure is properly indicated and performed. Bonardi et al.4 report their experience with 144 patients submitted to the Whitehead technique, with postoperative complaints related to difficult anal hygiene (72%), bleeding (60%), wet anus (49%) and anal burning (27%). The main complications were: bleeding in two patients, asymptomatic stenosis in two patients and anal skin tags in five patients.
RBL of internal hemorrhoids associated with surgical resection of external hemorrhoids (Santos4,27)
Santos4,27 has used RBL as the treatment of choice for internal hemorrhoids since 1980, with a series of 3,000 patients, totaling around 10,000 ligations. A high incidence of external hemorrhoids or anal skin tags in his patients, subsequently requiring resections of external parts, combined with the concepts of anatomical constitution of the anal canal floor, have made Santos, since 1986, indicate what he has called "hybrid hemorrhoidectomy": conventional RBL for the eradication of internal hemorrhoids and external hemorrhoidectomy or plicomectomy for the eradication of external hemorrhoids of the HD, at the same time. In addition, Santos4,27 considered studies conducted by Barron3 (about RBL) and Parks25 (about submucosal hemorrhoidectomy), in which tissues were surgically resected by submucosal dissection, as an option to preserve, even partially, the anal canal floor integrity.
Mechanical anopexy with circular clamp (Longo6)
In late 1990's, Longo6 described a new surgical method to treat HD without hemorrhoid resection, but using mechanical anopexy with circular clamp adapted to this procedure. The PPH removes an annular and circular portion of the mucosa and submucosa from the region above the pectineal line, lifting and fixing the hemorrhoidal vessels that would also interrupt blood flow in case of persistent external hemorrhoids. According to the concept itself, the technique is not a hemorrhoidectomy, but a hemorrhoidopexy. But, based on the studies and results of Longo, other surgeons4,12,31 started to study this new method, its results and complications. Personal alterations have been made, such as that made by Regadas4. Several series have been reported.
Surgical complications of hemorrhoidectomy
When discussing the complications resulting from hemorrhoidectomy, the opinions of authors are different: some include postoperative symptoms (for instance: pain, urinary retention, bleeding, incontinence, intestinal constipation and stool becoming hard and dry), which are eliminated still at the hospital by taking clinical measures. Other authors include systemic occurrences from concomitant diseases and conditions presented by the patients in the preoperative period and that are not directly associated with hemorrhoidectomy, but with the surgical action or anesthesia (for instance: hypertensive crisis, myocardial infarction, cephalalgia, hyperglycemia, hypoglycemia, vomiting, various types of thromboembolism, sepsis of various origins, including urinary infections caused by the use of vesical probes). On the other hand, some mention anal occurrences that appear until 1 month after the surgery as postoperative complications: stenosis, local sepsis (for instance, abscess, infection and fistula), thrombosis, bleeding, worsening of anal hypotonia and fecal incontinence. Other authors also mention the low degree of patient satisfaction one year after the surgery (for instance: presence of anal skin tags, difficult defecation, anal burning after evacuation, stool becoming thinner and involuntary farting). It causes very difficult comparison of cases using the same techniques and different techniques to treat the disease. This study considers that anal complications are exclusively anal occurrences related to the surgery itself and that cannot be resolved through clinical measures: anal stenosis (Figure 3), anal bleeding, anal sepsis (abscess and infection) and worsening of anal hypotonia. Then, in "Discussion", this study avoids the use of statistical data and findings of other authors that were not in the present series of cases.
OBJECTIVES
The objective of this study is to analyze and update 87 cases of surgical complications resulting from a series of 2,840 patients submitted to hemorrhoidectomy using Milligan-Morgan, Ferguson and mixed techniques along the period of 46 years of professional activity of this specialty (1965 to 2011), analyzing:
1. incidence of HD and hemorrhoidectomy by gender of patients; the incidence of HD and hemorrhoidectomy by age groups of patients; hemorrhoidectomy techniques used in 2,840 patients; incidence of complications from the surgical techniques employed in 2,840 hemorrhoidectomy procedures; hemorrhoidectomy complications by gender of patients; hemorrhoidectomy complications by age groups of patients; distribution of 50 cases of anal stenosis by the type of anal tone, by the occurrence of not of anal fissure and by its anatomical shape (annular, semi-annular and tubular); distribution of 50 cases of anal stenosis by gender and age groups of patients; surgical techniques used in 50 cases of anal stenosis, results and recurrences; diagnosis and approach of 23 cases of anal bleeding, seven cases of worsening of anal hypotonia, severe anal sepsis and systemic complications.
Series of cases patients and method
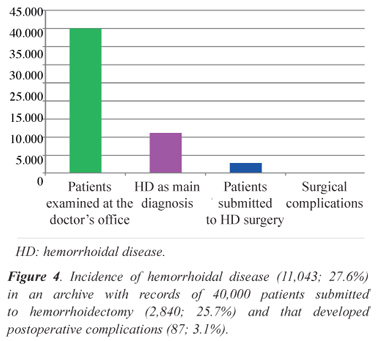
Along 46 years of practice fully centered on Coloproctology, the author had the opportunity to keep records from 40,000 patients, having diagnosed HD as the underlying disease and reason for doctor's visit in 11,043 patients (27.6%), with 2,840 (25.7%) of them submitted to hemorrhoidectomy, resulting in 87 surgical complications (Table 1 and Figure 4). This study refers to these 87 complications.
RESULTS
Incidence of HD and hemorrhoidectomy in 40,000 patients analyzed
Among total 40,000 patients examined, HD was diagnosed as the reason for doctor's visit in 11,043 patients (27.6%), with 2,840 (25.7%) of them submitted to hemorrhoidectomy (Table 1 and Figures 4 and 5).
Incidence of HD by gender of patients
HD was more common in women (5,945 cases; 53.8%) than men (5,108 cases; 46.2%), considering total 11,043 patients diagnosed with HD.
Incidence of hemorrhoidectomy by gender of patients
Among total 2,840 patients submitted to surgery for HD, 1,573 were female patients (55.4%) and 1,267 were male patients (44.6%). From a total of 5,945 women with HD, 1,573 were submitted to the surgical procedure (26.5%) and from 5,108 men with HD, 1,267 (24.8%) were submitted to surgical procedure (Table 3 and Figure 6).
Incidence of HD by age groups of patients
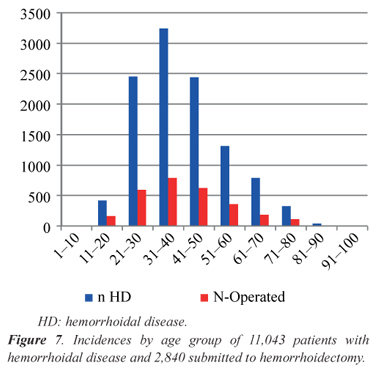
The fourth decade of life (31 to 40 years of age) was the most prevalent, with 3,243 cases (29.4%), followed by the third (2,451 cases; 22.2%) and fifth decades (2,442 cases; 22.1%), with these three age groups accounting for 8,136 patients (73.7%). The other 26.3% were distributed as follows: sixth (1,318 cases; 11.9%), seventh (791 cases; 7.1%), second (422 cases; 3.8%), eighth (329 cases; 3.0%) and ninth (38 cases; 0.4%) decades. Regarding hemorrhoidectomy, the incidences had similar results to age groups at the diagnosis: the fourth decade was the most prevalent (786 cases; 27.7%), followed by the fifth (622 cases; 21.9%) and the third (596 cases; 21.0%) decades, and the other age groups.
Incidence of hemorrhoidectomy by age groups of patients:
The distribution of 2,840 patients submitted to HD surgery in relation to their age groups was the following: of 422 patients between 11 and 20 years old with HD, 161 (38.2%) were submitted to the surgery; as well as 596 of 2,421 patients between 21 and 30 years old (24.3%); 786 of 3,243 patients between 31 and 40 years old (24.2%); 622 of 2,442 patients between 41 and 50 years old (25.5%); 362 of 1,318 patients between 51 and 60 years old (27.5%); 182 of 791 patients between 61 and 70 years old (23.0%); 118 of 329 patients between 71 and 80 years old (35.9%); and 13 of 38 patients between 81 and 90 years old (34.5%) (Table 4 and Figure 7).
Hemorrhoidectomy techniques used in 2,840 patients submitted to surgical procedure
From total 2,840 patients undergoing hemorrhoidectomy, most of them (2,189 cases, 77.1%) were submitted to the open technique of Milligan-Morgan, followed by the closed technique of Ferguson (341 cases, 12.0%) and mixed techniques open and closed methods (310 cases, 10.9%) (Table 5 and Figure 8).
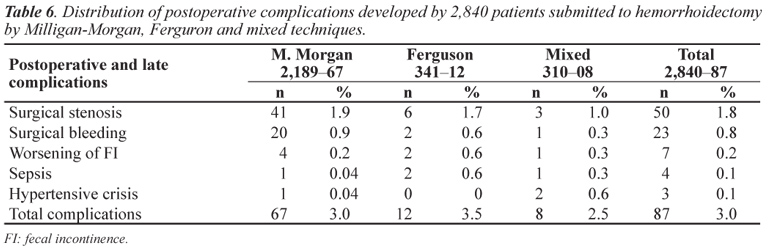
Incidence of complications from surgical techniques employed in 2,840 hemorrhoidectomy procedures
In total, 87 surgical complications (3.0%) were observed in 2,840 hemorrhoidectomy procedures. From 2,189 patients submitted to hemorrhoidectomy by the open technique of Milligan-Morgan, 67 (3.0%) developed the following surgical complications: stenosis (41 cases; 1.9%), severe bleeding (20 cases, 1.9%), worsening of anal hypotonia (four cases; 0.2%) and others (1 case, 0.04% severe hypertensive crisis with anal bleeding). From 341 patients submitted to hemorrhoidectomy by the closed technique of Ferguson, 12 (3.5%) developed the following surgical complications: stenosis (6 cases; 1.7%), severe bleeding (2 cases, 0.6%), worsening of anal hypotonia (2 cases; 0.6%) and sepsis (2 cases, 0.6%). From 310 patients submitted to hemorrhoidectomy by mixed techniques (closed and open methods), eight (2.5%) developed the following surgical complications: stenosis (3 cases; 1.0%), severe bleeding (1 case, 0.3%), worsening of anal hypotonia (1 case, 0.3%), sepsis (1 case, 0.3%) and others (1 case of hypertensive crisis with anal bleeding and 1 case of anaphylactic shock with cardiac arrest and resuscitation during the surgery, 0.3%). From 2,840 patients undergoing the 3 techniques, 87 (3.0%) had surgical complications: 50 cases of anal stenosis (1.8%), 23 cases of severe bleeding (0.8%), 7 cases of worsening of anal hypotonia (0,2%), 4 cases of sepsis (0.1%) and others (3 cases, 0.1%) (Table 6 and Figures 9 and 10).
Complications and types of complications from 2,840 hemorrhoidectomy procedures by gender of patients
In total, 87 surgical complications (3.1%) were observed in 2,840 hemorrhoidectomy procedures, 46 of them in women (3.0%). The main complications were: 50 cases (1.8%) of anal stenosis (31 women, 2.0%; 19 men, 1.5%), 23 cases (0.8%) of severe bleeding (9 women, 0.6%; 14 men, 1.1%), 7 cases (0.2%) of worsening of anal hypotonia (6 women; 0.4%), 4 cases (0.2%) of sepsis (no woman; 4 men, 0.3%) and 3 cases (0.1%) of other complications (no woman; 3 men, 0.2%, specifically 2 cases of hypertensive crisis with surgical bleeding and 1 case of anaphylactic shock with cardiac arrest and resuscitation) (Table 7 and Figures 11 and 12).
Complications and types of complications from 2,840 hemorrhoidectomy procedures by age groups of patients
In total, 87 surgical complications (3.1%) were observed in 2,840 hemorrhoidectomy procedures, with the following distribution in terms of age groups of patients: in 161 hemorrhoidectomy procedures performed in the second decade of life, four complications (2.5%) occurred, all cases of anal stenosis (5; 2.5%). In 596 hemorrhoidectomy procedures in the third decade, 20 complications (3.4%) occurred: 14 cases of stenosis (2.3%) and 6 cases of bleeding (1.0%). In 786 hemorrhoidectomy procedures in the fourth decade, 27 complications (3.4%) occurred: 18 cases of stenosis (2.3%) and 6 cases of bleeding (0.8%), 2 cases of worsening of anal hypotonia (0.2%) and 1 anal sepsis (0.1%). In 622 hemorrhoidectomy procedures in the fifth decade, 15 complications (2.4%) occurred: 9 cases of stenosis (1.4%), 5 cases of bleeding (0.8%) and 1 case of worsening of anal hypotonia (0.2%). In 362 hemorrhoidectomy procedures in the sixth decade, 8 complications (2.2%) occurred: 4 cases of stenosis (1.1%), 3 cases of bleeding (0.8%) and 1 systemic complication (hypertensive crisis with anal bleeding) (0.3%). In 182 hemorrhoidectomy procedures in the seventh decade, 7 complications (3.8%) occurred: 1 case of stenosis (1.5%), 2 cases of bleeding (1.1%), 1 case of worsening of anal hypotonia (0.5%), 1 case of sepsis (0.5%) and 2 cases of systemic complications - 1 hypertensive crisis with anal bleeding and 1 anaphylactic shock with cardiac arrest and resuscitation (1.1%). In 118 hemorrhoidectomy procedures in the eighth decade, 6 complications (5.1%) occurred: 1 case of stenosis (0.8%), 1 case of bleeding (0.8%), 3 cases of worsening of anal hypotonia (2.5%), and 2 cases of anal sepsis (1.1%). In 13 hemorrhoidectomy procedures in the ninth decade, no complication occurred (Table 8 and Figures 13 and 14).
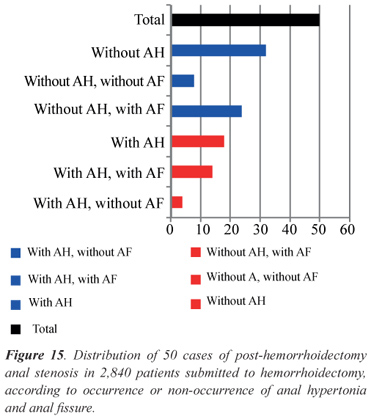
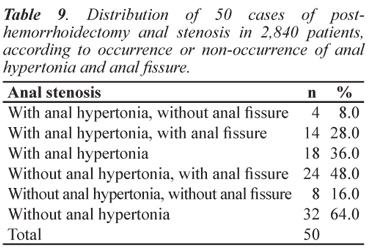
Distribution of 50 cases of post-hemorrhoidectomy anal stenosis by the type of anal tone and occurrence or non-occurrence of anal fissure from 2,840 hemorrhoidectomy procedures
The proctologic exam was limited to the inspection and, in most cases, to the unsuccessful attempt to perform the digital rectal exam, even if with the small finger. Then, the findings of the proctologic exam refer, in a considerable number of patients, to findings at the moment of surgery, with the patient already sedated. These findings (Table 9 and Figures 15 and 16) were sorted according to two observations: sphincter tone (with and without sphincter hypertonia) and anal fissure (with and without anal fissure). Regarding the anal tone, anal hypertonia occurred in 18 patients (36.0%): 14 (28.0%) with anal fissure and 4 (8.0%) without anal fissure; and anal hypertonia in 32 patients (64.0%): 24 with anal fissure (48.0%) and 8 without anal fissure (16.0%).
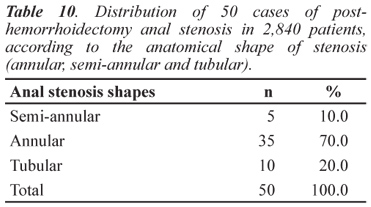
Distribution of 50 cases of post-hemorrhoidectomy anal stenosis by the anatomical shape (annular, semi-annular and tubular) from 2,840 hemorrhoidectomy procedures
Regarding the stenosis extension and shape, most cases of stenosis were annular (35 cases, 70.0%), followed by tubular stenosis (10 cases, 20.0%) and semi-annular (5 cases, 10.0%) (Table 10 and Figure 17).
Distribution of 50 cases of post-hemorrhoidectomy anal stenosis by gender from 2,840 hemorrhoidectomy procedures
Among 1,573 women submitted to hemorrhoidectomy, 31 (2.0%) developed anal stenosis; and among 1,267 men, 19 (1.5%) developed anal stenosis (Table 11 and Figure 18).
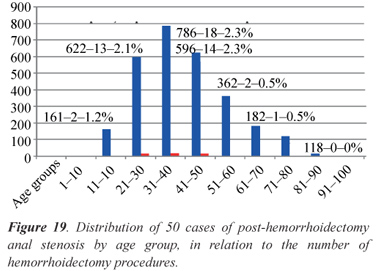
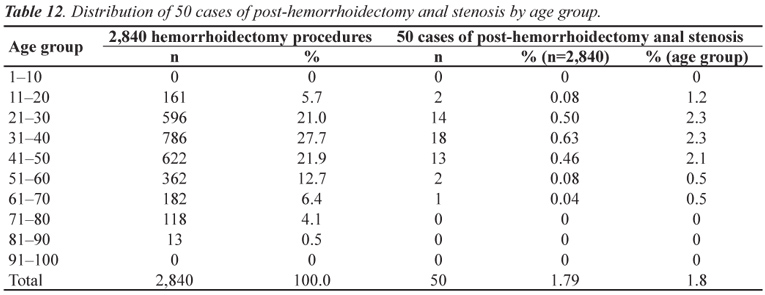
Distribution of 50 cases of post-hemorrhoidectomy anal stenosis by age groups from 2,840 hemorrhoidectomy procedures
Post-hemorrhoidectomy anal stenosis occurred in 50 patients: 2 were in the second decade of life (1.2%), 14 in the third (2.3%), 18 in the fourth (2.3%), 13 in the fifth (2.1%), 2 in the sixth (0.5%) and 1 in the seventh (0.5%) decades. The mean age of incidence of anal stenosis in these 50 patients was 38.2 years (Table 12 and Figure 19).
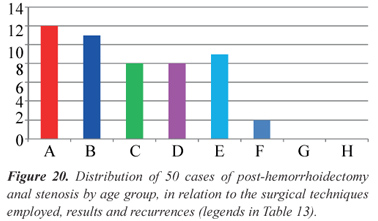
Distribution of 50 cases of post-hemorrhoidectomy anal stenosis by surgical techniques employed, results and recurrence rates from 2,840 hemorrhoidectomy procedures
The various surgical techniques used in 50 patients with post-hemorrhoidectomy anal stenosis were (Table 13 and Figure 20): 12 patients (24.0%) were submitted to single anotomy and excision of fibrotic area without sphincterotomy; 11 patients (22.0%) were submitted to dual anotomy and excision of fibrotic area without sphincterotomy; 8 patients (16.0%) were submitted to simple anotomy and excision of fibrotic area with internal sphincterotomy (and the subcutaneous portion of the external sphincter); 8 patients (16.0%) were submitted to dual anotomy and excision of fibrotic area with internal sphincterotomy (and the subcutaneous portion of the external sphincter); 9 patients (18.0%) were submitted to anoplasty with V-shaped cutaneous flap; 2 patients (4.0%) were submitted to anoplasty with rectangular cutaneous flap; and no case was observed of anoplasty with mucosal flap or mucosal lowering and anoplasty with dual flap or mixed flap or cutaneous and mucosal flaps. The incidence of anal stenosis recurrence related to the techniques employed was 8.0% (four cases): two recurrences (4.0%) with the use of "single anotomy and excision of fibrotic area without sphincterotomy"; one recurrence (2.0%) with the use of "dual anotomy and excision of fibrotic area without sphincterotomy"; and one recurrence (2.0%) with the use of "anoplasty with V-shaped cutaneous flap. Regarding the incidence of anal stenosis by technique employed, the results were the following: 2 recurrences (16.7%) in single anotomy with excision of fibrotic area and fissurectomy without sphincterotomy; 1 recurrence (9.1%) in 11 dual anotomy procedures with excision of fibrotic area and fissurectomy without sphincterotomy; and 1 recurrence (11.1%) in 9 anoplasty procedures with V-shaped flap (Table 13 and Figure 20).
Distribution of 23 cases of post-hemorrhoidectomy anal bleeding from 2,840 hemorrhoidectomy procedures
Of 2,840 patients submitted to hemorrhoidectomy, 23 (0.8%) developed severe anal bleeding, which required surgical intervention, and all were submitted to transfixation of pedicles ligated at the underlying surgery (Table 14).
Distribution of 7 cases of worsening of anal hypotonia (fecal incontinence) from 2,840 hemorrhoidectomy procedures
Of 2,840 patients submitted to hemorrhoidectomy, 7 (0.2%) presented strong worsening of fecal incontinence (Table 15).
Severe anal sepsis from 2,840 patients submitted to hemorrhoidectomy
Of 2,840 patients submitted to hemorrhoidectomy, 4 (0.1%) developed severe anal sepsis, all treated with debridement and antibioticotherapy, no death.
Hypertensive crisis and arrhythmia from 2,840 patients submitted to hemorrhoidectomy
Of 2,840 patients submitted to hemorrhoidectomy, 3 presented cardiovascular occurrences: 2 cases of hypertensive crisis and 1 case of severe arrhythmia, all resolved, no death.
DISCUSSION
Complications from hemorrhoidectomy by open technique Milligan-Morgan
Arbman et al.10, in a series of 39 hemorrhoidectomy procedures by the open technique, observed complications in 5 patients: 4 cases of bleeding and 1 case of worsening of anal hypotonia. They also reported recurrent HD in 10% of the patients 12 months after the surgery.
1. Cruz et al.2,4,32, in a partial series of 2,014 patients submitted to hemorrhoidectomy procedures by the open technique, reported 61 cases of surgical complications (3.0%): 38 cases of anal stenosis (1.9%), 19 cases of bleeding (0.9%), 3 cases of worsening of anal hypotonia (0.1%) and 1 case of systemic complication (0.05%).
2. Complications from hemorrhoidectomy by closed technique Ferguson
3. The largest series of closed hemorrhoidectomy (Ferguson) in the medical literature was reported by Ganchrow et al.11: 2,038 patients were submitted to this surgery, and the authors classified postoperative complications as postoperative (82 cases, 4.0%) and late (99 cases, 4.8%), including systemic complications, from pneumonia to cystitis. Considering anal complications only, the following incidences were observed: anal fissure (54 cases; 2.7%), anal stenosis (24 cases; 1.2%), surgical bleeding (27 cases; 1.3%), anal abscess (17 cases; 0.8%), anal fistula (5 cases; 0.2%), totaling 127 anal complications (6.2%).
4. However, without the series described by Ganchrow et al.11, postoperative complications from hemorrhoidectomy by the closed technique of Ferguson are not more than 5% of incidence reported in the medical literature, a fact mentioned by Senagore et al.30 and Khubchandani et al.16, with the main occurrences: stenosis, bleeding, infection, recurrence, late healing, anal fissure, anal incontinence and fistulas.
Another interesting series using the closed technique is reported by McConnell and Khubchandani17,18, who analyzed 441 patients submitted to closed hemorrhoidectomy, with follow-up between 1 and 7 years. Unfortunately, they did not distinguish postoperative from late complications, which produced indices reaching 7.5%, exceeding the maximum acceptable limit of 5.0%.
Cruz et al. (2006)2,4,32, in a partial series of 232 patients submitted to closed hemorrhoidectomy, reported 8 cases of surgical complications (3.4%): 4 cases of anal stenosis (1.7%), 1 case of bleeding (0.4%), 1 case of worsening of anal hypotonia (0.4%) and 2 cases of sepsis (0.9%).
In a series of 514 patients submitted to closed hemorrhoidectomy, Guenin et al.15 observed only 9 cases of complications (1.8%): 7 cases of bleeding and 2 cases of occasional soiling (0.9%), who were submitted to a new surgery. The degree of satisfaction of those patients analyzed up to 7 years in the follow-up period, was considered excellent (70.5%) and good (87%), which made these authors consider the closed technique of Ferguson as the "golden standard", to which other techniques should be compared.
Complications from hemorrhoidectomy by both techniques, by the same author
Arbman et al.9, in a series of 77 hemorrhoidectomy procedures by open technique (39 cases) and closed technique (38 cases), observed complications in 5 patients submitted to the open technique and no patient submitted to the closed technique. They also reported recurrent HD in 10% of the patients 12 months after the surgery, by both techniques. They concluded that "both methods are comparable, although healing after closed hemorrhoidectomy is faster and causes less bleeding". The study cannot be deeply analyzed, as N is very low to allow any conclusion.
You et al.33, in a series of 80 patients submitted to hemorrhoidectomy by both closed and open techniques, did not report any complication, but they observed that less intense pain in the group submitted to closed hemorrhoidectomy, in which healing was faster (75% in 3 weeks) versus open hemorrhoidectomy (18% in 3 weeks).
Cruz et al.2,4,32, in a series of 2,014 patients submitted to open hemorrhoidectomy, reported 61 cases of surgical complications (3.0%): 38 cases of anal stenosis (1.9%), 19 cases of bleeding (0.9%), 3 cases of worsening of anal hypotonia (0.1%) and 1 case of systemic complication (0.05%). Also Cruz et al.2,4,32, in a series of 232 patients submitted to closed hemorrhoidectomy, reported 8 cases of surgical complications (3.4%): 4 cases of anal stenosis (1.7%), 1 case of bleeding (0.4%), 1 case of worsening of anal hypotonia (0.4%) and 2 cases of sepsis (0.9%). Then, these authors have not obtained results indicating superiority of either technique.
While some authors, such as Arbman et al.10, Guenin et al.16 and You et al.33, using both techniques, demonstrate in their series of cases that the closed technique bring better results than the open technique, either with or without statistical significance, other authors, such as Gençosmanoglu et al.34, Carapeti et al.15, Ho and Ho5 and Wolfe et al.35, based on their comparative series, say that the open technique is better than the closed technique. Others2,4,32 say that there is no difference between both techniques in terms of incidence of complications.
Comparison between two large series of open and closed hemorrhoidectomy, by two authors
The most recent series analyzing the largest number of patients submitted to Milligan-Morgan hemorrhoidectomy is the partial series of Cruz et al.2,4,32, in a large personal series, with 2,417 hemorrhoidectomy procedures performed: 2,014 by the open technique (Milligan-Morgan), 232 by the closed technique (Ferguson) and 171 by mixed techniques (open and closed procedures). According to these authors2,4,32, of 2,014 surgeries by the open technique, 55 anal complications (2.7%) were observed: 38 cases of anal stenosis (1.9%), 9 cases of bleeding (0.4%) and 8 other complications (0.4%); and, of 232 surgeries by the closed technique, 7 complications (3.0%) were observed: 4 cases of stenosis (1.7%), 1 case of bleeding (0.4%) and 2 other complications (0.9%); and, of 171 surgeries using mixed techniques, 4 complications (2.4%) were observed: 2 cases of stenosis (1.2%), 1 case of bleeding (0.6%) and 1 case of sepsis (0.6%). Then, this series did not show a statistically significant difference in terms of postoperative complications when comparing both (open and closed) techniques. The largest series of closed hemorrhoidectomy (Ferguson) in the medical literature was reported by Ganchrow et al.11: 2,038 patients were submitted to this surgery, and the authors classified postoperative complications as postoperative (82 cases, 4.0%) and late (99 cases, 4.8%), including systemic complications, from pneumonia to cystitis. Considering anal complications only, the following incidences were observed: anal fissure (54 cases; 2.7%), anal stenosis (24 cases; 1.2%), surgical bleeding (27 cases; 1.3%), anal abscess (17 cases; 0.8%), anal fistula (5 cases; 0.2%), totaling 127 anal complications (6.2%). When comparing the series of 2,014 patients submitted to open hemorrhoidectomy (Milligan-Morgan) of Cruz et al.2,4,32 with the series of 2,038 patients submitted to closed hemorrhoidectomy (Ferguson) of Ganchrow et al.11, the incidence of complications in the open technique was exactly half (76 cases; 3.1%) of the number reported in the closed technique (127 cases; 6.2%).
Hemorrhoidectomy by mixed techniques (closed and open techniques):
We found no other reference to this practice in the medical literature, except for the series reported by Cruz et al.2,4,32, who submitted 171 patients with HD to mixed technique, resulting in 4 complications (2.4%): 2 cases of stenosis (1.2%), 1 base of bleeding (0.6%) and 1 case of worsening of anal hypotonia (0.6%).
Comparison of incidences of complications from hemorrhoidectomy by open, closed and mixed techniques, in this series of patients and related to other series
The final series presented in this study is a series of 2,840 hemorrhoidectomy procedures by Milligan-Morgan technique (2,189 cases), Ferguson technique (341 cases) and mixed techniques (310 cases) in 11,043 patients with HD. The series observed 67 complications in 2,189 hemorrhoidectomy procedures by Milligan-Morgan technique (3.0%): stenosis (41 cases; 1.9%), severe bleeding (20 cases; 1.9%), worsening of anal hypotonia (4 cases; 0.2%) and others (1 case of severe hypertensive crisis with anal bleeding; 0.04%). The series observed 12 complications in 341 hemorrhoidectomy procedures by Ferguson technique (3.5%): stenosis (6 cases; 1.7%), severe bleeding (2 cases; 0.6%), worsening of anal hypotonia (2 cases; 0.6%) and sepsis (2 cases; 0.6%). The series observed 8 complications (2.5%) in 310 hemorrhoidectomy procedures by mixed techniques (open and closed techniques): stenosis (3 cases; 1.0%), severe bleeding (1 case; 0.3%), worsening of anal hypotonia (1 case; 0.3%), sepsis (1 case; 0.3%) and others (1 case of hypertensive crisis with anal bleeding and 1 case of anaphylactic shock with cardiac arrest and resuscitation; 0.3%). No statistical difference in the incidence of complications was observed when comparing the three techniques employed. When comparing the incidences of complications in this series to other studies in the medical literature, the results from the open technique are better in this series, comparable in terms of closed technique, and, regarding mixed techniques, no comparison was made, due to unavailable information on this theme in the literature.
CONCLUSIONS
Follow-up in the series of 2,840 hemorrhoidectomy procedures by Milligan-Morgan technique (2,189 cases), Ferguson (341 cases) and mixed (310 cases) in 11,043 patients with HD allowed the following conclusions:
the acceptance of surgical indication for HD by the patients was 25.7%; HD was more common in women than men and hemorrhoidectomy was better accepted by women than men (p<0.05); hemorrhoidectomy was performed more often in patients in the fourth, fifth and third decades of life. The patients that better accepted the surgical indication were in the second, eighth and ninth decades of life; the overall incidence of surgical complications was 3.0%; the most common complications were: anal stenosis and severe bleeding, with no difference between the surgical techniques employed; complications affected more women (p>0.05), with higher incidence of stenosis in women (p<0.05); complications affected more patients in the eighth and seventh decades of life (p<0.05); the most common anal stenosis was without anal hypertonia and with anal fissure, and its most common anatomic shape was annular (70.0%); anal stenosis was more common in women, mean age of 38.2 years, no relation to age groups; the most frequently used corrective surgery of anal stenosis was single anotomy with or without fissurectomy and without sphincterotomy; all cases of anal bleeding had surgical ligation of all hemorrhoidal pedicles, no matter if the bleeding site was found or not.
Submitted on: 03/13/2012
Approved on: 06/14/2012
Conflict of interest: nothing to declare.
References
- 1. Thomson WHF. The nature of haemorrhoids. Br J Surgery 1975;62(7):542-52.
- 2. Cruz GMG. Santana JL, Santana SKAA, Ferreira RMRS, neves pm, Faria MNZ. Hemorroidectomia: estudo de 2.417 pacientes submetidos à cirurgia para tratamento de doença hemorroidária. Rev Bras Coloproct 2006;26(3):253-68.
- 3. Barron J. Office ligation treatment of hemorrhoids. Dis Col Rectum 1963;6:109-13.
- 4. Cruz GMG. Doença hemorroidária. São Caetano do Sul, SP: Yendis, 2008.
- 5. Ho KS, Ho YH. Prospective randomized trial comparing stapled hemorrhoidopexy versus closed Ferguson hemorrhoidectomy. Tech Coloproctol 2006;10(3):193-7.
- 6. Longo A. Anopexia mecânica com grampeador (PPH). Treatment of hemorrhoid disease by reduction of mucosa and haemorrhoidal prolapse with a Circular Suturing Device A New Procedure. In: Sixth World Congress of Endoscopic Surgery, 1998, Rome, Italy; 1998. p. 777-90.
- 7. Seixas IV, Pupo Neto JA. Hemorroidectomia com bisturi harmônico. Hospital dos Servidores do Estado e Mestrado, UFRJ, RJ. Pôster 22, suplementos da Revista Brasileira de Alergia e Imunopatologia.
- 8. Milligan ETC, Morgan CN. Surgical anatomy of the anal canal and the operative treatment of hemorrhoids. Lancet II. 1937;1119-24.
- 9. Andrews BT, Layer GT, Jackson BT, Nichols RJ. Randomized trial comparing diathermy hemorrhoidectomy with the scissor dissection Milligan-Morgan operation. Dis Colon Rectum 1993;36(6):580-3.
- 10. Arbman G, Krook H, Haapaniemi S. Closed vs. open hemorrhoidectomy--is there any difference? Dis Colon Rectum 2000;43(1):31-4.
- 11. Ganchrow MI, Mazier WP, Friend WG, Ferguson JA. Hemorrhoidectomy revisited a computer analysis of 2.038 cases. Dis Colon Rectum 1971;14(2):128-33.
- 12. Ho YH, Seow-Choen F, Tan M, Leong AF. Randomized controlled trial of open and closed hemorrhoidectomy. Brit J Surg 1997;84(12):1729-30.
- 13. Pandini LC, Nahas SC, Nahas CSR, Marques CFS, Sobrado CW, Kiss DR. Surgical treatment of haemorrhoidal disease with CO2 laser and Milligan-Morgan cold scalpel technique. Colorectal Dis 2006;8(7):592-5.
- 14. Ferguson JA, Heaton JR. Closed hemorrhoidectomy. Dis Colon Rectum 1959;2(2):176-9.
- 15. Carapeti EA, Kamm MA, McDonald PJ, Phillips RK. Randomized trial of open versus closed day-case hemorrhoidectomy. Br J Surg 1999;86(5):612-3. Comments in: Br J Surg 2001;88(11):1547-8.
- 16. Guenin MO, Rosenthal R, Kern B, Peterli R, von Flue M, Ackermann C. Ferguson hemorrhoidectomy: long-term results and patient satisfaction after Ferguson's hemorrhoidectomy. Dis Colon Rectum 2005;48(8):1523-7.
- 17. Khubchandani IT, Trimpi HD, Sheets JA. Closed hemorrhoidectomy with local anesthesia. Surg Gynecol Obstet 1972;135(6):955-7.
- 18. McConnell JC, Khubchandani IT. Long-term follow-up of closed hemorrhoidectomy. Dis Colon Rectum 1983;26(12):797-9.
- 19. Whitehead W. The surgical treatment of haemorrhoids. Br Med J 1882;1(1101):148-50.
- 20. Whitehead W. Three hundred consecutive cases of haemorrhoids cured by excision. Br Med J (Clin Res) 1887;1(1365):449-51.
- 21. Wollf G, Culp CE. The Whitehead hemorrhoidectomy. An unjustly maligned procedure. Dis Colon Rectum 1988;31(8):567-9.
- 22. Borba MR, Sobrado Jr CW, Sokol S. Hemorroidectomia pela técnica fechada (Técnica de Sokol) Análise de 322 doentes. Rev Bras Coloproct 1977;17(2):98-100.
- 23. Ruiz-Moreno F. Hemorrhoidectomy--how I do it: semiclosed technique. Dis Colon Rectum 1977;20(3):177-82.
- 24. Obando RN. Hemorrhoids. An Alap 1966;1:110.
- 25. Parks AG. The surgical treatment of haemorrhoids. Br J Surg 1956;43(180):337-51.
- 26. Milito G, Cortese F, Brancaleone C, Casciani CU. Submucosal hemorrhoidectomy surgical results and complications in 1315 patients. Techniques in coloproctology 1997;1:128-32.
- 27. Santos HA. Hemorroidectomia híbrida. uma nova abordagem no tratamento das hemorróidas mistas. Rev Bras Coloproct 2006;4(28):377-88.
- 28. Iwagaki H, Higuchi Y, Fuchimoto S, Orita K. The laser treatment of hemorrhoids: results of a study on 1,816 patients. Jpn J Surg 1989;19(6):658-61.
- 29. Zahir KS, Edwards RE, Vecchia A, Dudrick SJ, Tripodi G. Use of the Nd-YAG laser improves quality of life and economic factors in the treatment of hemorrhoids. Conn Med 2000;64(4):199-203.
- 30. Tan JJY, Seow-Choen F. Prospective, randomized trial comparing diathermy and harmonic scalpel hemorrhoidectomy. Dis. Colon Rectum 2001;44(5):677-9.
- 31. Senagore AJ, Singer M, Abcarian H, Fleshman J, Corman M, Wexner S et al. Procedure for Prolapse and Hemorrhoids (PPH) Multicenter Study Group. A prospective, randomized, controlled multicenter trial comparing stapled hemorrhoidopexy and Ferguson hemorrhoidectomy: perioperative and one-year results. Dis Colon Rectum 2004;47(11):1824-36.
- 32. Cruz GMG, Santana SKAA, Santana JL, Ferreira RMRS, Neves PM, Faria MNZ. Complicações pós-operatórias cirúrgicas da hemorroidectomia: revisão de 76 casos de complicações. Rev Bras Coloproct 2007;27(1):42-57.
- 33. You SY, Kim SH, Chung CS, Lee DK. Open vs. closed hemorrhoidectomy. Dis Colon Rectum 2005;48(1):108-13.
- 34. Gençosmanoglu R, Sad O, Koc D, Inceoglu R. Hemorrhoidectomy: open or closed technique? A prospective, randomized clinical trial. Dis Colon Rectum 2002;45 (1):70-5.
- 35. Wolfe JS, Muñoz JJ, Rocín JD. Survey of hemorrhoidectomy practices: open versus closed techniques. Dis Colon Rectum 1979;22:536-8.
Publication Dates
-
Publication in this collection
08 Jan 2013 -
Date of issue
Sept 2012
History
-
Received
13 Mar 2012 -
Accepted
14 June 2012
 Surgical complications in 2,840 cases of hemorrhoidectomy by Milligan-Morgan, Ferguson and combined techniques
Surgical complications in 2,840 cases of hemorrhoidectomy by Milligan-Morgan, Ferguson and combined techniques