Abstracts
PURPOSE: To describe the fluoroscopic findings of swallowing in preterm infants with zero to six months of age, as well as the related diseases and clinical signs and symptoms, and to compare these findings with data obtained from full-term infants. METHODS: The retrospective findings of fluoroscopic studies carried out in infants with zero to six months of age and their respective files were analyzed. Participants were 40 subjects divided into two groups: Preterm Group, composed by 23 preterm infants, and Full-Term Group, with 17 infants born full-term. RESULTS: Nasopharyngeal and gastroesophageal reflux were the main fluoroscopic findings of swallowing in both groups. There was no difference between the groups regarding the presence of swallowing disorders. The Preterm Group presented more cardiac problems than the Full-Term Group. No differences were found between the groups regarding neurologic and respiratory problems. With respect to clinical signs and symptoms suggestive of swallowing disorders, the Preterm Group presented more oxygen desaturation and the Full-Term Group, more vomiting. CONCLUSION: Nasopharyngeal reflux and gastroesophageal reflux were the main fluoroscopic findings of swallowing in preterm infants with zero to six months of age. New follow-up studies with this population must be carried out to confirm the hypothesis that the swallowing alterations observed were due to immaturity in the swallowing function.
Fluoroscopy; Infant; newborn; Infant; premature; Deglutition disorders; Gastroesophageal reflux
OBJETIVO: Descrever os achados fluoroscópicos da deglutição de recém-nascidos pré-termo de zero a seis meses de idade, assim como as doenças e os sinais e sintomas clínicos relacionados à alteração na deglutição, e compará-los com os respectivos dados obtidos de recém-nascidos de termo. MÉTODOS: Foram analisados, retrospectivamente, os dados das avaliações fluoroscópicas realizadas no período de um ano em lactentes de zero a seis meses de idade e aos respectivos prontuários. Participaram 40 sujeitos, divididos em dois grupos: Grupo Pré-Termo, constituído de 23 recém-nascidos pré-termo; e Grupo de Termo, constituído por 17 recém-nascidos de termo. RESULTADOS: Os principais achados fluoroscópicos da deglutição observados em ambos os grupos foram refluxo para a nasofaringe e refluxo gastresofágico. Não houve diferença entre os grupos para a presença de alteração na deglutição . O Grupo Pré-Termo apresentou mais problemas cardíacos do que o Grupo de Termo. Não houve diferença entre os grupos para problemas neurológicos e respiratórios. Em relação aos sinais e sintomas clínicos sugestivos de alteração na deglutição, o Grupo Pré-Termo apresentou mais dessaturação de oxigênio e o Grupo de Termo mais vômitos. CONCLUSÃO: Os principais achados fluoroscópicos da deglutição encontrados em recém-nascidos pré-termo de zero a seis meses de idade foram refluxo para a nasofaringe e refluxo gastresofágico. Novos estudos de seguimento desta população devem ser realizados para confirmar a hipótese de que as alterações na deglutição observadas ocorreram devido à imaturidade na função de deglutição.
Fluoroscopia; Recém-nascido; Prematuro; Transtornos de deglutição; Refluxo gastresofágico
ORIGINAL ARTICLE ARTIGO ORIGINAL
Fluoroscopic findings of swallowing: comparison between preterm and full-term infants
Lenice de Fatima da Silva-MunhozI ; Karina Elena Bernadis BühlerII
ISchool of Medicine, Universidade de São Paulo USP São Paulo (SP), Brazil
IIUniversity Hospital, Universidade de São Paulo USP São Paulo (SP), Brazil
Correspondence address
ABSTRACT
PURPOSE: To describe the fluoroscopic findings of swallowing in preterm infants with zero to six months of age, as well as the related diseases and clinical signs and symptoms, and to compare these findings with data obtained from full-term infants.
METHODS: The retrospective findings of fluoroscopic studies carried out in infants with zero to six months of age and their respective files were analyzed. Participants were 40 subjects divided into two groups: Preterm Group, composed by 23 preterm infants, and Full-Term Group, with 17 infants born full-term.
RESULTS: Nasopharyngeal and gastroesophageal reflux were the main fluoroscopic findings of swallowing in both groups. There was no difference between the groups regarding the presence of swallowing disorders. The Preterm Group presented more cardiac problems than the Full-Term Group. No differences were found between the groups regarding neurologic and respiratory problems. With respect to clinical signs and symptoms suggestive of swallowing disorders, the Preterm Group presented more oxygen desaturation and the Full-Term Group, more vomiting.
CONCLUSION: Nasopharyngeal reflux and gastroesophageal reflux were the main fluoroscopic findings of swallowing in preterm infants with zero to six months of age. New follow-up studies with this population must be carried out to confirm the hypothesis that the swallowing alterations observed were due to immaturity in the swallowing function.
Keywords: Fluoroscopy, Infant, newborn, Infant, premature, Deglutition disorders, Gastroesophageal reflux
INTRODUCTION
The establishment of neonatal intensive care units, allied to the technological development of obstetric and perinatal medicine, has resulted in the increase of survival rates for high-risk infants, especially in the last two decades(1). With greater survival, studies have emphasized the evaluation of neonatal morbidity and its consequences, especially in preterm newborns (PTNB)(2).
Literature reports that PTNB, besides being more likely to develop neurological, cardiac and/or respiratory alterations, can also present swallowing disorders(3). However, there are few studies describing swallowing alterations in this population using fluoroscopic assessment.
Oral feeding in newborn infants is a complex activity that requires efficient coordination of sucking, breathing and swallowing functions so that there is no effort and/or risk for aspiration(4). Nevertheless, this coordination becomes possible only around the 32nd to the 34th week gestational age(4,5), although the 34th is frequently used as minimum expectation for enough oral ingestion to reach water and nutritional needs(6). Usually, the exclusive oral feeding ability is reached after the 37th week gestational age(7).
In PTNB, sucking, swallowing and breathing coordination might be impaired both because of neurological immaturity or the presence of cardiac and/or respiratory conditions. Moreover, abnormal muscle tone, altered oral reflexes, and difficulty to regulate organization states can difficult their performance regarding oral and swallowing abilities(8,9).
Hence, PTNB require alternative feeding methods until they acquire the abilities needed for oral feeding(7). However, prolonged dependence of alternative feeding increases the possibility of sensory deprivation and jeopardizes the early development of feeding, interrupting sequences of appetitive ingestive behaviors that compose important learning experiences(9).
Many PTNB present respiratory problems that require oxygen support. The development of rhythmic oral patterns for sucking might be impaired in these infants, who are constantly subjected to abnormal tactile stimulation in perioral and intraoral sensitive tissues during periods of endotracheal intubation and use of continuous positive airway pressure(4).
Sucking-swallowing-breathing coordination is obtained when the infant can safely and efficiently receive oral feeding, that is, with no risk of aspiration. This coordination is evidenced by the absence of alteration in physiological parameters, such as oxygen desaturation, respiratory discomfort, apnea, bradycardia or tachycardia, and demonstration of 1:1:1 or 2:2:1 ratio for sucking to swallowing to breathing(4).
During feeding, PTNB are notably less efficient than full-term newborns (FTNB), presenting failures and alternative efforts to protect their airways and periods of apnea during vigorous sucking, which prevent them from presenting the consistent 1:1:1 sequence of sucking, swallowing and breathing observed among FTNB(8). Hence, during oral feeding, this population can present episodes of desaturation, apnea and/or bradycardia(4), which are clinical signs suggestive of alterations in swallowing dynamics.
The main signs and symptoms that can indicate deglutition disorders are: weight loss, refusal to feed, irritation, cough, regurgitation, choking, respiratory discomfort, stridor, cyanosis, apnea, oxygen desaturation, bradycardia, and recurrent respiratory infections, especially pneumonia(10-12). In these cases, the following swallowing phases can be altered: oral preparatory, oral, pharyngeal and/or esophageal(10). Moreover, these signs and symptoms can also indicate the presence of gastroesophageal reflux (GER)(13,14).
The incidence of GER in PTNB varies from 22% to 85%(13). The pharyngeal stimulation due to GER episodes, in PTNB, causes the reflex interruption of breathing and bradycardia instead of swallowing and cough, as in FTNB(15). A few studies have tried to demonstrate the relationship between the presence of GER, apnea and bradycardia on PTNB, however, the results are controversial: some show correlation between them(15,16), while others do not corroborate these findings(17,18).
Videofluoroscopy is the gold standard method of objective swallowing assessment. It allows the assessment of both structures and details regarding swallowing phases and the dynamics between them, which is not possible based only in clinical assessment. Thus, it can be observed: velopharyngeal competence, pharyngeal transit time, premature spillage and/or stasis of food in the valleculae or piriform sinuses laryngeal elevation, and laryngeal penetration and/or aspiration before, during or after swallowing (silent or not). The bolus transit from the esophagus to the stomach can also be observed, and the presence of GER can be detected, as well as laryngeal penetration and/or aspiration of gastric content(6,10,11,19,20).
Temporal measures of the events related to the dynamics of swallowing, such as oral transit time, onset of pharyngeal closure, time of bolus arrival at the valleculae, pharyngeal delay, pharyngeal transit and upper esophageal sphincter (UES) opening, can also be obtained with videofluoroscopy. These measures can help the identification of swallowing disorders and the elaboration of an adequate therapeutic planning. However, there are only few studies that evaluate these measures with the aim to standardize them for use in pediatric population(21).
Swallowing disorders with aspiration are a common cause of difficulties related to feeding in infancy(12). Studies have showed that videofluoroscopy is a method able to detect aspiration, silent or not, and to appropriately identify the swallowing alterations, which allow therapeutic planning and the establishment of compensatory mechanisms(12,22,23).
Abnormal videofluoroscopy results in newborns include nasopharyngeal reflux, laryngeal penetration and aspiration, with a high incidence of silent aspiration. This emphasizes the importance of objective swallowing assessment for this population(20).
Children with respiratory problems may present swallowing alterations, which can be observed in videofluoroscopic evaluation(22,24-26). According to some authors, swallowing disorders are frequently observed in infants with history of bronchitis and/or recurrent pneumonia. Moreover, these disorders might be the cause of the respiratory symptoms in this population(22).
In a study with infants with pneumonia, it was verified correlation between the condition and the presence of residue in the pharynx after swallowing, the aspiration of liquids, and gastroesophageal reflux disease (GERD)(24). Another study showed that swallowing disorders characterized by aspiration occurred in the acute phase of bronchiolitis in previously healthy children, even though they did not present clinical signs of such alterations(25).
In a study with infants with no apparent risk factors associated to swallowing and respiratory problems without cause, it was observed swallowing alterations characterized by delay in the onset of the pharyngeal phase. In this study, the delay always preceded penetration or laryngeal aspiration, and all aspirations were silent. Hence, oropharyngeal disphagia must be considered in the differential diagnosis of this population(26).
In infants with severe neurological disorders, alterations in oral and pharyngeal phases of swallowing, which result in aspiration, are the main cause of respiratory infections(11). Children with GERD can also present swallowing disorders and feeding difficulties. Authors have conducted videofluoroscopy in 11 children with GERD, and observed predominance of alterations in oral preparatory and oral phases, especially with solid food. They also verified silent aspiration in 18.2% of the children, and delay in esophageal transit in 36.4%(27).
GER associated to aspiration can increase the incidence of respiratory infections. A previous study has shown that children with severe neurological disorders associated to GER and aspiration are more prone to severe respiratory infections. GER with swallowing disorders that do not result in aspiration has less risk to cause respiratory infections in this population(11).
As in adults, children who suffered traumatic brain injury can present swallowing disorders in the acute phase. Authors have studied the videofluoroscopic results of 18 children in the acute phase after moderate/severe traumatic brain injury, and observed the following alterations: reduced lingual control, lingual hesitation movements, presence of aspiration (including silent aspiration), delay in triggering swallowing reflex, reduced laryngeal closure and elevation, and decreased peristaltic movement(28).
Based on the aforementioned, it is evident the need for videofluoroscopy evaluation in children with signs and symptoms indicative of swallowing disorders, with the aim to objectively characterize them and, hence, outline an adequate therapeutic planning. No studies focusing specifically on fluoroscopic evaluation in PTNB were found.
Therefore, the aim of the present study was to describe the fluoroscopic findings of swallowing of zero- to six-month-old PTNB, as well as the diseases and clinical signs and symptoms related to the swallowing disorders, and to compare these data to that of FTNB.
METHODS
This study was approved by the Research Ethics Committee of the University Hospital of Universidade de São Paulo (HU-USP), under process number 830/08. It was carried out a retrospective analysis of data from fluoroscopic evaluations conducted at the Radiology sector of the hospital in the period between September/2007 and September/2008, in infants from zero to six months old. The following data were gathered from subjects' records: date of birth, gestational age (GA), birth
weight (BW), gender, peri- and postnatal complications, diseases and clinical signs and symptoms suggestive of alterations in oral, pharyngeal and esophageal phases of swallowing (reason for indication of fluoroscopic assessment).
The diseases observed were divided into three groups: neurological problems (mild/moderate perinatal asphyxia, hydrocephalus, and traumatic brain injury), cardiac problems (patent foramen ovale, patent ductus arteriosus, and functional murmur), and respiratory problems, which were subdivided into specific diagnoses (early respiratory distress, pulmonary bronchodysplasia, respiratory distress syndrome, hyaline membrane disease, bronchiolitis, bronchopneumonia, chronic laryngitis, and vocal fold paresis) and clinical signs (apnea, cough, dyspnea, stridor, prolonged expiratory phase, and wheezing. Possible history and duration of endotracheal intubation was also considered as respiratory problems.
The records of zero- to six-month-old infants submitted to fluoroscopic evaluation in the period from September/2007 to September/2008 in the Radiology sector of the University Hospital were included. Exclusion criteria eliminated the records of infants that did not present oral and/or pharyngeal phases of swallowing during the fluoroscopic assessment due to the presence of craniofacial abnormalities, genetic syndromes, severe perinatal asphyxia, and/or use of alternative feeding, and the records of evaluations with unavailable results at the hospital's archive system.
In the period considered, 44 zero- to six-month-old infants were submitted to fluoroscopic assessment. However, four were excluded because they did not correspond to the criteria adopted in this study.
The 40 records included were divided into two groups: Preterm Group (PTG), composed of 23 PTNB (mean GA = 32.5 weeks; mean BW = 1,805 g); and Full Term Group (FTG), composed of 17 FTNB (mean GA = 39.7 weeks; mean BW = 3,211 g). The minimum chronological age was four days, and the maximum, five months and 19 days. Corrected ages of PTNB were not considered.
Evaluations were carried out using the equipment Phillips® DuoDiagnostic, collimated to the area of interest, with exposition parameters automatically defined by an ionization camera, where the best fluoroscopic image is obtained with lower doses of radiation. To record the fluoroscopy, infants were positioned in elevated decubitus with compression belt, allowing secure retention, and in lateral vision, as close as possible to the table top and the intensifier, avoiding distortions of the fluoroscopic image.
Contrast was offered in orthodontic nipples NUK® with hole for thin liquid; it was used a 50% dilution of barium sulfate at 100% (Bariogel®) and 50% of warm milk, with the total volume prescribed by the neonatologist. The focus of the fluoroscopic image in the anterior region was delimited by the lips, in the superior region by the nasal cavity, in the posterior region by the cervical spine, and in the inferior region by the bifurcation of the airway and the cervical esophagus. For the GER study, infants were positioned in supine position, with a waiting time of approximately five minutes, using intermittent scopy, with the aim to obtain the lowest radiologic exposure possible.
The following conditions were considered swallowing alterations in the fluoroscopic evaluation: presence of contrast in the nasopharynx during swallowing, presence of residue in the piriform sinuses, laryngeal penetration, and laryngotracheal aspiration. It was also observed the possible presence and site of GER.
Statistical analysis used the Test for Equality of Two Proportions for comparisons between groups, and the Fisher Exact Test to verify the association between swallowing, GER, diseases and clinical signs and symptoms related to swallowing disorders. It was adopted a significance level of 0.05.
RESULTS
The PTG presented greater frequency of cardiac problems than the FTG (p=0.040). No differences were found between groups for neurological and respiratory problems. When specific diagnoses were considered, there were differences in the PTG for the following respiratory problems: early respiratory distress (p=0.012), bronchodysplasia (p=0.012), and apnea (p=0.040).
In the comparison between groups regarding clinical signs and symptoms suggestive of swallowing disorders and GER, the PTG presented more occurrence of oxygen desaturation (p=0.001) and the FTG, of vomits (p=0.038). Only the PTG presented nausea, bradycardia, respiratory distress and sucking difficulties; only the FTG presented choking and nasal obstruction. These signs were observed in the groups separately. There were no differences between groups regarding cyanosis, regurgitation, cough, poor appetite, and apnea (Table 1).
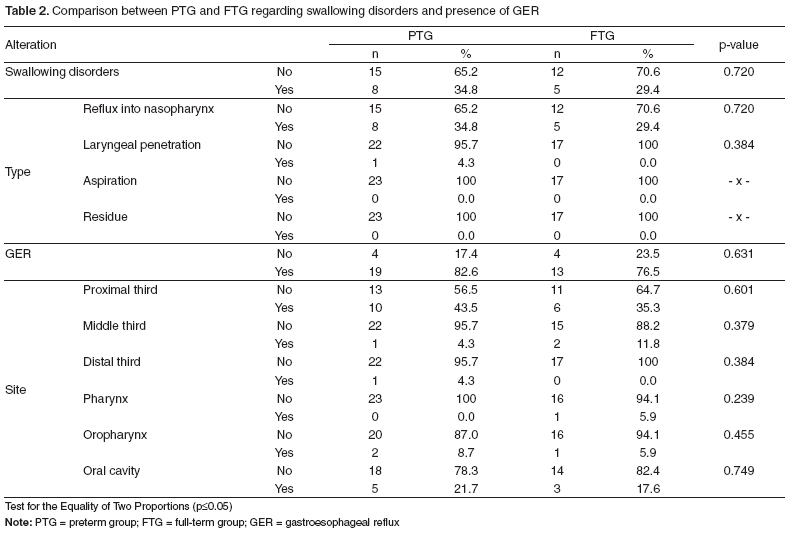
No differences were found between groups also with regards to the presence of alterations during the oral and pharyngeal phases of swallowing (p=0.720) and the presence of GER (p=0.631). The main swallowing alteration found in both groups was reflux into the nasopharynx, and there were no observations of laryngotracheal aspiration or presence of residue in the piriform sinuses. Only one PTNB presented laryngeal penetration. There was higher occurrence of GER until the proximal third of the esophagus and until the oral cavity in both groups (Table 2).
Overall, 32.5% of the subjects presented swallowing disorders (reflux into nasopharynx = 100%, and laryngeal penetration = 7.7%) and 80% presented GER (predominant site at the proximal third of the esophagus = 50%, and until the oral cavity = 25%).
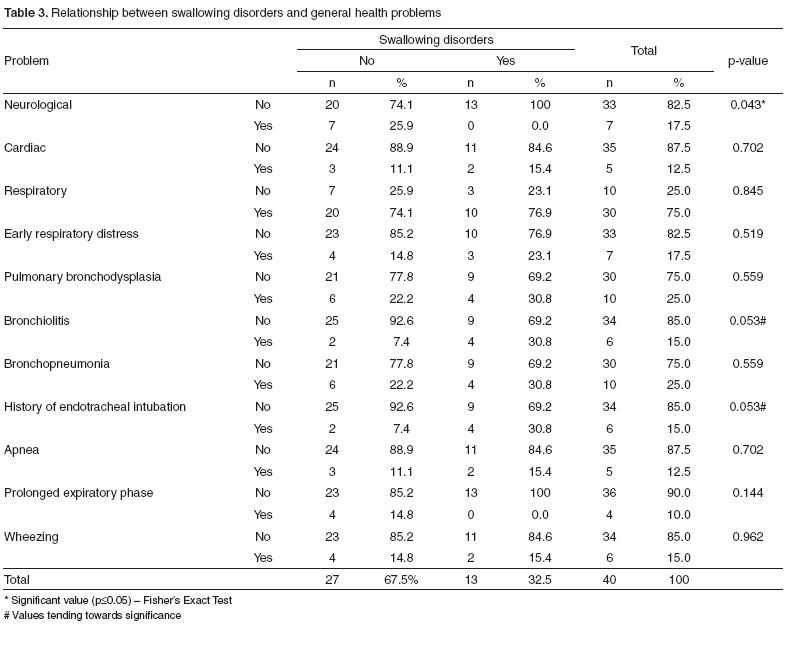
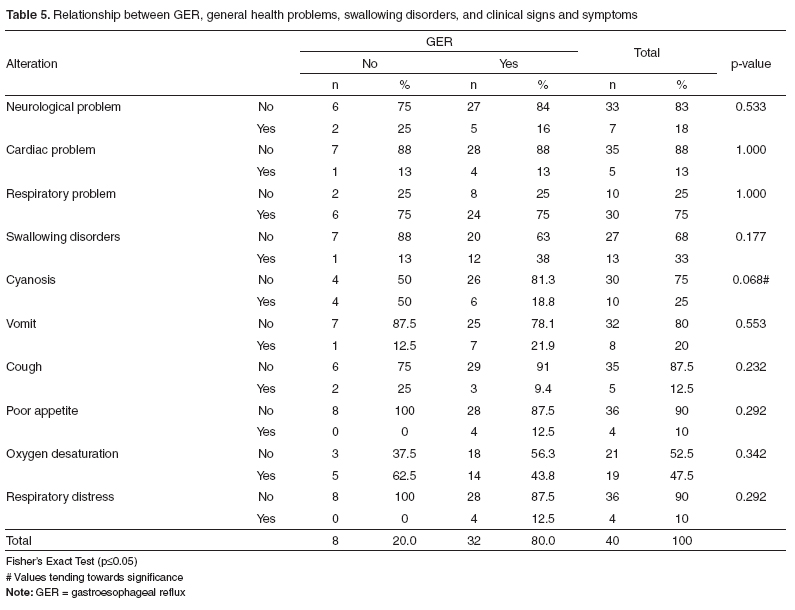
The verification of association between swallowing disorders and neurological, cardiac and respiratory problems (Table 3) and with clinical signs and symptoms (Table 4), showed differences for neurological problems (p=0.043). There was no association between alterations in oral and pharyngeal phases of swallowing and presence of GER (Table 5). There was no association between the presence of GER and neurological, cardiac and respiratory problems, nor between GER and clinical signs and symptoms.
DISCUSSION
In the present study, the main swallowing disorders observed in both groups were reflux into the nasopharynx and gastroesophageal reflux. The reflux into the nasopharynx signals swallowing incoordination during the pharyngeal phase, caused by inefficient elevation of the soft palate. Because newborns are obrigatory nasal breathers, the increase of secretions in the nasopharynx due to this alteration might difficult the sucking-swallowing rhythm(22).
Some authors consider that minimal refluxes into the nasopharynx and laryngeal penetrations are normal in newborns, because these alterations can be physiological in this population, due to swallowing immaturity(12). Therefore, it can be considered that the reflux into the nasopharynx observed in the subjects of the present study was due to swallowing immaturity, which caused swallowing incoordination. However, new studies, especially follow-up studies with this population, must be conducted to confirm this hypothesis.
Sucking-swallowing-breathing incoordination can cause laryngotracheal aspiration and/or penetration in newborns(22). In PTNB, it can occur due to neurological immaturity and the presence of cardiac and/or respiratory problems(8). In the present study, only one PTNB presented laryngeal penetration.
The occurrence of GER in children is frequent, especially in the first 18 months of age, when the immaturity controlling swallowing phases and coordinating peristaltic waves is evident(29). We found a high incidence of GER in the studied population (80%), which corroborates literature data(13,29).
Children with GER can present alterations in the oral and pharyngeal phases of swallowing and feeding difficulties(27). However, in the present study, the presence of GER was not related to alterations in the oral and pharyngeal phases of swallowing.
In this study, the PTNB presented more cardiac problems than FTNB. Moreover, it was observed higher frequencies of early respiratory distress, bronchodysplasia and episodes of apnea in this population. These data corroborate studies that show that PTNB are more prone to presenting such problems(3).
The clinical signs and symptoms that motivated the indication of fluoroscopic evaluation in this study were the same described in literature(10-14). The higher incidence of oxygen desaturation, bradycardia and respiratory distress in PTNB might be due to the frequent respiratory and cardiac problems, to the incoordination between sucking, swallowing and breathing related to prematurity(4,7), or to the high incidence of GER, even though there are still controversies regarding the relationship between GER and clinical signs and symptoms(15-18).
The sucking difficulties observed only in PTNB can be related to their neurological immaturity, as described in literature(8). It is believed that the nasal obstruction observed in two FTNB are due to both the reflux into the nasopharynx verified in the fluoroscopic assessment and the presence of respiratory problems.
Vomit after feeding is one of the manifestations of GER(30). In the present study, there was higher incidence of vomit among FTNB. When clinical signs and symptoms were correlated with alterations in the oral and pharyngeal phases of swallowing and GER, no difference was found. Literature shows that GER can stimulate receptors located especially at the pharynx and larynx, triggering reflex mechanisms that might cause acute cardiorespiratory symptoms, such as bronchospasm, laryngospasm, central apnea and bradycardia, which can cause cyanosis(29).
Moreover, there was difference in the relation between swallowing disorder and neurological problems. Children with neurological alterations, including traumatic brain injury, can present swallowing disorders(11,28).
CONCLUSION
The main fluoroscopic findings of swallowing in zero- to six-month-old PTNB were reflux into the nasopharynx and gastroesophageal reflux. This population presented more cardiac problems than FTNB. Regarding the clinical signs and symptoms related to swallowing disorders, the PTNB presented more incidence of oxygen desaturation.
The speech-language pathologist must be alert during swallowing assessments of PTNB and/or newborns with neurological, respiratory and/or cardiac problems, for these are the risk factors for swallowing disorders. Whenever possible and advised, clinical assessment should be complemented with fluoroscopic evaluation.
Further follow-up studies must be conducted with this population to confirm the hypothesis that the swallowing disorders observed in the present study were due to swallowing function immaturity. Moreover, new prospective studies with larger samples must be carried out for better understanding of normal physiology of swallowing in infants.
REFERENCES
- 1. Markestad T, Kaaresen PI, Rřnnestad A, Reigstad H, Lossius K, Medbř S, et al. Zanussi. Early death, morbidity, and need of treatment among extremely premature infants. Pediatrics. 2005;115(5):1289-98.
- 2. Rugolo LM. Growth and developmental outcomes of the extremely preterm infant. J Pediatr (Rio J). 2005;81(1Suppl):S101-10.
- 3. Leone CR, Tronchin DM. Assistência integrada ao recém-nascido. São Paulo: Atheneu; 2001.
- 4. Barlow SM. Oral and respiratory control for preterm feeding. Curr Opin Otolaryngol Head Neck Surg. 2009;17(3):179-86.
- 5. Madureira DL. Deglutição em neonatos. In: Ferreira LP, Befi-Lopes DM, Limongi SCO. Tratado de fonoaudiologia. São Paulo: Roca; 2004. p. 219-29.
- 6. Delaney AL, Arvedson JC. Development of swallowing and feeding: prenatal through first year of life. Dev Disabil Res Rev. 2008;14(2):105-17.
- 7. Salinas-Valdebenito L, Núñez-Farias AC, Milagros A, Escobar-Henríquez RG. Caracterización clínica y evolución trás la intervención terapêutica de trastornos de deglución en pacientes pediátricos hospitalizados. Rev Neurol. 2010;50(3):139-44.
- 8. Xavier C. Intervenção fonoaudiológica em bebês de risco. In: Ferreira LP, Befi-Lopes DM, Limongi SCO. Tratado de fonoaudiologia. São Paulo: Roca; 2004. p. 415-38.
- 9. Bingham PM. Deprivation and dysphagia in premature infants. J Child Neurol. 2009:24(6):743-9.
- 10. Darrow DH, Harley CM. Evaluation of swallowing disorders in children. Otolaryngol Clin North Am. 1998;31(3):405-18.
- 11. Morton RE, Wheatley R, Minford J. Respiratory tract infections due to direct and reflux aspiration in children with severe neurodisability. Dev Med Child Neurol. 1999;41(5):329-34.
- 12. Vazquez JL, Buonomo C. Feeding difficulties in the first days of life: findings on upper gastrointestinal series and the role of the videofluoroscopic swallowing study. Pediatr Radiol. 1999;29(12):894-6.
- 13. Tipnis NA, Tipnis SM. Controversies in the treatment of gastroesophageal reflux disease in preterm infants. Clin Perinatol. 2009;36(1):153-64.
- 14. Tighe MP, Beattie RM. Managing gastro-oesophageal reflux in infancy. Arch Dis Child. 2010;95(4):243-4.
- 15. Paul K, Melichar J, Miletín J, Dittrichová J. Differential diagnosis of apneas in preterm infants. Eur J Pediatr. 2009;168(2):195-201.
- 16. Corvaglia L, Zama D, Gualdi S, Ferlini M, Aceti A, Faldella G. Gastro-oesophageal reflux increases the number of apnoeas in very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2009;94(3):F188-92.
- 17. Slocum C, Arko M, Di Fiore J, Martin RJ, Hibbs AM. Apnea, bradycardia and desaturation in preterm infants before and after feeding. J Perinatol. 2009;29(3):209-12.
- 18. Wheatley E, Kennedy KA. Cross-over trial of treatment for bradycardia attributed to gastroesophageal reflux in preterm infants. J Pediatr. 2009:155(4):516-21.
- 19. Miller CK, Willging JP. Advances in the evaluation and management of pediatric dysphagia. Curr Opin Otolaryngol Head Neck Surg. 2003;11(6):442-6.
- 20. Hiorns MP, Ryan MM. Current practice in paediatric videofluoroscopy. Pediatr Radiol. 2006;36(9):911-9.
- 21. Weckmueller J, Easterling C, Arvedson J. Preliminary temporal measurement analysis of normal oropharyngeal swallowing in infants and young children. Dysphagia. 2010;26(2):135-43.
- 22. Mercado-Deane MG, Burton EM, Harlow AS, Glover AS, Deane DA, Guill MF, et al. Swallowing dysfunction in infants less than 1 year of age. Pediatr Radiol. 2001;31(6):423-8.
- 23. Silva AB, Piovesana AM, Barcelos IH, Capellini SA. Evaluación clínica y videofluoroscópica de la deglución em pacientes con parálisis cerebral tetraparésica espástica y atetósica. Rev Neurol. 2006;42(8):462-5.
- 24. Weir K, McMahon S, Barry L, Ware R, Masters IB, Chang AB. Oropharyngeal aspiration and pneumonia in children. Pediatr Pulmonol. 2007;42(11):1024-31.
- 25. Khoshoo V, Edell D. Previously healthy infants may have increased risk of aspiration during respiratory syncytial viral bronchiolitis. Pediatrics. 1999;104(6):1389-90.
- 26. Lefton-Greif MA, Carroll JL, Loughlin GM. Long-term follow-up of oropharyngeal dysphagia in children without apparent risk factors. Pediatr Pulmonol. 2006;41(11):1040-8.
- 27. Mathisen B, Worrall L, Masel J, Wall C, Shepherd RW. Feeding problems in infants with gastro-oesophageal reflux disease: a controlled study. J Paediatr Child Health. 1999;35(2):163-9.
- 28. Morgan A, Ward E, Murdoch B, Bilbie K. Acute characteristics of pediatric dysphagia subsequent to traumatic brain injury: videofluoroscopic assessment. J Head Trauma Rehabil. 2002;17(3):220-41.
- 29. Fernandes AF. Refluxo gastresofágico em crianças. In: Costa HO, Duprat AC, Eckley CA. Laringologia pediátrica. São Paulo: Roca; 1999. p.181-202.
- 30. Duca AP, Dantas RO, Rodrigues AA, Sawamura R. Evaluation of swallowing in children with vomiting after feeding. Dysphagia. 2008;23(2):177-82.
Publication Dates
-
Publication in this collection
14 Oct 2011 -
Date of issue
Sept 2011
History
-
Received
05 Feb 2010 -
Accepted
28 Oct 2010