Abstracts
The author reports a case of focal acral hyperkeratosis, an affection of the group of keratodermas, characterized by papular or plaque eruption in the palmoplantar borders whose onset is usually before 20 years of age, and predominates among black-skinned patients. The main differential diagnosis is acrokeratoelastoidosis of Costa, differing from the former only for not presenting elastorrhexis in histopathology.
Keratin; Keratoderma palmoplantar; Keratoderma palmoplantar; Keratosis
O autor relata um caso de hiperceratose focal acral, afecção do grupo das ceratodermias marginais caracterizada por erupção papulosa ou em placa nas bordas palmoplantares que se inicia geralmente antes dos 20 anos de idade, com predomínio na raça negra. Seu principal diagnóstico diferencial é a acroceratoelastoidose de Costa que dela se distingue apenas por não apresentar elastorrexe na histopatologia.
Ceratodermia palmar e plantar; Ceratodermia palmar e plantar; Ceratose; Queratina
CASE REPORT
Focal acral hyperkeratosis: case report and discussion on marginal keratodermas* * Work done at Discipline of Dermatology at Faculdade de Medicina da Fundação ABC - Santo André (SP), Brazil. Conflict of interest: None.
Maurício Zanini
Specialist in Dermatology, member of the Brazilian Society of Dermatology
Mailing address Mailing address: Maurício Zanini Rua Marechal Floriano Peixoto, 245 Sala 87 89010-500 - Blumenau SC - Brazil Tel.: +55 47 3326-5326 E-mail: drzanini@terra.com.br
ABSTRACT
The author reports a case of focal acral hyperkeratosis, an affection of the group of keratodermas, characterized by papular or plaque eruption in the palmoplantar borders whose onset is usually before 20 years of age, and predominates among black-skinned patients. The main differential diagnosis is acrokeratoelastoidosis of Costa, differing from the former only for not presenting elastorrhexis in histopathology.
Keywords: Keratin/genetic; Keratoderma palmoplantar/classification; Keratoderma palmoplantar/diagnosis; Keratosis
INTRODUCTION
Palmoplantar keratoderma syndrome is characterized by palm and/or sole skin thickening, and may be either acquired or hereditary. There are three clinical presentations, according to lesion distribution: diffuse, focal and punctate.1,2 The author reports a case of focal acral hyperkeratosis, a form of punctate keratoderma, which, owing to the characteristic affection of hands and feet borders, it is also called marginal palmoplantar keratoderma.1
CASE REPORT
Twenty-year-old male patient, student, phototype IV, who had complained of warts in the hands for two years. Eruption was asymptomatic and had slow evolution. He had no important past medical history and denied similar cases in the family.
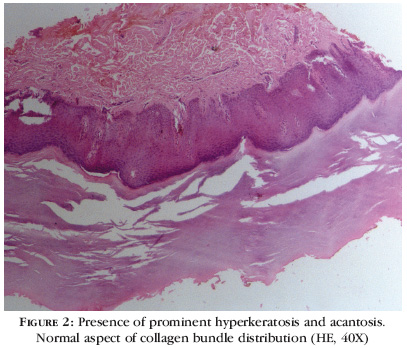
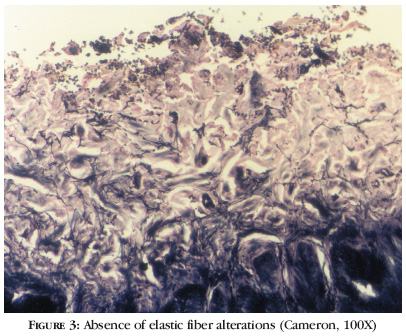
Upon dermatological examination, he presented, in the junction of dorsal and ventral surfaces of the hands, multiple oval and polygonal bright keratotic papules, which coalesced, forming plaques (Figure 1). Considered diagnostic hypotheses were papular annular granuloma, acrokeratoelastoidosis of Costa, acrokeratosis verruciformis of Hopf and plane wart. Histopathological examination showed marked hyperkeratosis, but no papilomatosis was observed, neither were elastic fiber alterations in Cameron stain (Figures 2 and 3).
Considering clinical and histopathological findings, diagnosis of focal acral hyperkeratosis was established, with ensuing treatment with salicylic acid cream at 8%, associated with urea 10%, alternated with retinoic acid cream at 0.05%, Patient presented no improvement after six months of treatment, leading to a expectant treatment.
DISCUSSION
Marginal keratodermas are characterized by affecting palmoplantar borders or transitions, but may also occur inversely to that, when affecting dorsa of the hands and/or feet. Entities belonging to this group are numerous, the main ones being acrokeratoelastoidosis of Costa, focal acral hyperkeratosis, degenerative collagenous plaque of the hand and acrokeratosis verruciformis.3,4 There is no consensus on the correct definition and nosological position of these affections, and many described forms are simply clinical varieties of others.1 Mantoux's porokeratosis is usually mentioned as a marginal keratoderma; however, keratotic and crateriform lesions are not confined to marginal areas.1 On the other hand, marginal keratoelastoidosis of the hand probably represents a clinical form of degenerative collagenous plaque of the hand. Likewise, acrokeratoelastoidosis of Costa is more of a disorder in keratinization than an elastic fiber disorder.5 Some authors believe that focal acral hyperkeratosis is a clinical variety of acrokeratoelastoidosis of Costa. In fact, there is a lot of controversy sorrounding its definition, to the point that some authors state that there may be elastorrhexis in this affection.3,4
Focal acral hyperkeratosis, described for the first time by Dowd et al. In 1983, is a disorder of common keratinization. As most palmoplantar keratodermas, focal acral hyperkeratosis is generally inherited by dominant autosomic transmission, even though sporadic cases may occur. It is more frequent among black people, with onset of symptoms before age 20 in over 80% of instances.6 It is clinically identical to acrokeratoelastoidosis of Costa, from which it can only be differentiated by means of histopathological or ultra-structural studies. Focal acral hyperkeratosis, unlike acrokeratoelastoidosis, has histopathological alterations that are limited to the epidermis (hyperkeratosis and acantosis), and shows no elastic fiber alteration (elastorrhexis) in the reticular dermis. Collagen fibers are normal.3,6,7 Lesions are distributed throughout junctions between dorsal and ventral surfaces of the hands and/or feet, including fingers and toes. They are oval or polygonal keratotic papules, sometimes umbilicated, whose numbers increase progressively.5 Differential diagnosis includes acrokeratoelastoidosis of Costa, plane wart, acrokeratosis verruciformis of Hopf, colloid milium and xantoma.7 Recently, Gesau et al. reported a case of marginated punctate palmoplantar keratoderma because of dioxin intoxication, the latter being a halogen compound often used as herbicide.8 Arsenic keratosis and basocellular nevus syndrome should also be remembered. Some authors believe that many cases diagnosed as focal acral hyperkeratosis were actually cases of acroelastoidosis, for the identification of elastorrhexis is difficult in slices included in paraffin.3,6 Treatment of focal acral hyperkeratosis with emollients, keratolytic or keratoplastic agents is frustrating. Use of etretinate 50 mg/day has been proven effective, but the rule is relapse after treatment interruption.5
Acrokeratosis verruciformis, described by Hopf in 1931, is a rare genodermatosis of dominant autosomic inheritance, which usually manifests at birth or in the first years of life, although a few late onset cases are reported. It is characterized by plane, erythematic-brownish or normal colored verrucous plaques, located in hand and feet dorsa. It also includes punctate palm keratoses, and ungueal alterations are often. On optic microscopy, it presents papilomatosis, acantosis, hypergranulosis and hyperkeratosis.1,4
Acrokeratoelastoidosis, described by the illustrious Brazilian Oswaldo Costa in 1952,9 is a rare condition, clinically characterized by small non-confluent yellow or translucent and occasionally keratotic crateriform papules. The most characteristic clinical feature of this affection is location of the lesion.7 It is usually a discrete eruption that can affect finger borders, wrist and antero-inferior surface of the leg.5 Eruption is asymptomatic. Onset is generally between 20 and 30 years of age, but both an early (three years) and a late (47 years) onset cases are reported.7 The disease can be sporadic or be transmitted by dominant autosomic inheritance, probably linked to chromosome 2. Chronic trauma can be a causal agent, but its pathogeny remains unknown.5-7 Histopathological examination reveals focal hyperkeratosis, acantosis, hypergranulosis and elastorrhexis in variable degrees.3,6
Degenerative collagenous plaque of the hands, described by Burks in 1959, is a common disorder that occurs mainly over the 40 to 60 years age range, and is generally associated to advanced dermatoheliosis. It is characterized by yellow, waxy, coalescent keratotic papules located in the margins of fingers one to four and ulnar surface of the hands. Besides the papular eruption, actinic alterations can be observed. Papules can coalesce, forming a plaque that extends to the base of the fingers.7 Histological findings include degenerative plaques of collagen fibers and marked actinic degeneration, which allows differentiation from focal acral hyperkeratosis and acrokeratoelastoidosis.5-7 Altered fibers are grouped randomly, forming bundles that extend from lower papular to reticular dermis.7
Marginal keratoelastoidosis of the hands, described by Kocsard in 1964, is both clinically and histologically similar to degenerative collagenous plaque of the hand, and probably represents a clinical variety of this affection. It differs from it only for compromising the lateral border of the index finger and medial border of the thumb.5,7 It is believed to be the result of chronic recurrent trauma, as in hand workers. Histologically, hyperkeratosis, hypergranulosis, discrete acantosis and papillary vascular ectasia are observed.7
Ramos and Silva's palmar marginated keratoderma represents a form secondary to chronic recurrent trauma, solar elastosis and maybe a local circulation disorder. It is characterized by the presence of hyperkeratotic strips in the cubital and radial borders of the hands.10
The group of marginal keratodermas is constituted by diverse affections, many of them not distinct entities, but only clinical varieties. Focal acral hyperkeratosis is common disorder; however, since it is asymptomatic, it is not a frequent complaint, thus often goes unnoticed. This is why it is seldom reported in the literature. Probably, some cases of acrokeratoelastoidosis of Costa have been reported as focal acral hyperkeratosis, because microscopic identification of elastorrhexis is usually difficult.
REFERENCES
Received on May 29, 2003.
Approved by the Consultive Council and accepted for publication on July 06, 2006.
- 1. Griffiths WAD, Judge MR, Leigh IM. Disorders of keratinization. In: Rook A, Wilkinson DS, Ebling FJG. Textbook of Dermatology. 6 ed. Oxford: Blackwell Science; 1998. p.1483-588.
- 2. Stevens HP, Leigh IM. The inherited keratodermas of palms and soles. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz S, et al. Fitzpatrick's Dermatology in General Medicine. 5 ed. Philadelphia: MacGraw-Hill; 1998. p.604-12.
- 3. Rubegni P, De Aloe G, Romano C, Flori ML, Fimiani M. Acrokeratoelastoidosis: a report of two sporadic cases. Clin Exp Dermatol. 1997;22:54-64.
- 4. Rongioletti F, Betti R, Crosti Rebora A. Marginal papular acrokeratodermas: a unified nosography for focal acral hyperkeratosis, acrokeratoelastoidosis and related disorders. Dermatology. 1994;188:28-31.
- 5. Shbaklo Z, Jamaleddine NF, Kibbi AG, Salman SM, Zaynoun ST. Acrokeratoelastoidosis. Int J Dermatol. 1990;29:333-6.
- 6. Waxtein-Morgenstern L, Teixeira F, Cortes-Franco R, Veja-Memije ME, Ortiz-Plata A, Zamora-Hernandez C, Dominguez-Soto L. Lenticular acral keratosis in washer women. Int J Dermatol. 1998;37:532-7.
- 7. Nelson-Adesokan P, Mallory SB, Lombardi C, Lund R. Acrokeratoelastoidosis of Costa. Int J Dermatol. 1995;34:431-3.
- 8. Gesau A, Jurecka W, Nahavandi H, Schmidt JB, Stingl G, Tschachler E. Punctate keratoderma-like lesions on the palms and sole in a patient with chloracne: a new clinical manifestation of dioxin intoxication? Br J Dermatol. 2000;143:1067-71.
- 9. Costa OG. Acrokeratoelastosis. Arch Dermatol. 1954;70:228-31.
- 10. Sampaio SAP, Rivitti EA. Dermatologia. São Paulo: Artes Médicas; 1998. p.780-1.
Publication Dates
-
Publication in this collection
22 Dec 2006 -
Date of issue
Oct 2006
History
-
Accepted
06 July 2006 -
Received
29 May 2003